If you are staring at a low back pain X-ray report and thinking, “I still don’t know what this means,” you are not alone. A low back pain X-ray is one of the most commonly ordered first-line tests for back symptoms, but the language is written for clinicians, not for patients.
Most reports list what is visible (bones, alignment, spacing) without explaining what is not visible (discs, nerves, most soft tissues) or how strongly each finding relates to pain. This guide fills that gap from a patient perspective: what happens during the test, how the spine is “counted,” what common phrases usually mean, and why sacralization matters more than most people realize.

The simplest truth: what an X-ray is and is not
An X-ray is a picture made using a small dose of ionizing radiation. Dense structures—especially bone—block more X-rays and appear brighter/whiter. Less dense structures—muscles, ligaments, discs, and nerves—do not show well and may be essentially invisible.
So a low back pain X-ray is best viewed as a “bone and alignment test,” not a “pinpoint the pain source” test.
A low back pain X-ray is good at showing:
- Bone shape and bone injury (for example, fractures, compression)
- Alignment and curves (for example, scoliosis)
- Vertebra-to-vertebra position changes (for example, spondylolisthesis)
- Indirect clues about disc height (seen as disc space narrowing)
- Some congenital/anatomic variants (for example, sacralization)
A low back pain X-ray is not good at showing:
- Disc bulges, disc herniations, or disc tears (MRI is usually needed)
- Nerve compression (MRI is usually needed)
- Muscles, tendons, and many ligament injuries
- Many early infections, early tumors, or inflammatory changes
That gap—what you want to know vs what the test can show—is why reports can feel unsatisfying.
How many bones are in the low back, and how are they “counted”?
Most people want a straightforward answer: “How many bones do I have here, and what am I looking at?”
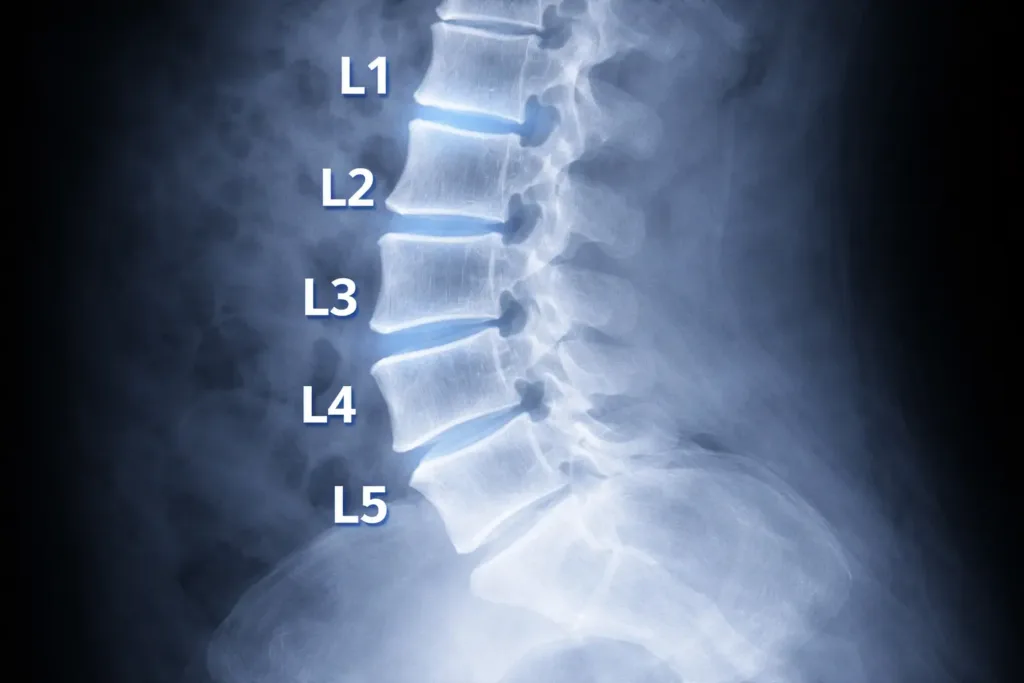
The lumbar spine: usually five vertebrae
The lumbar spine typically has five vertebrae: L1, L2, L3, L4, and L5. They sit between the rib-bearing thoracic spine (T12 is just above L1) and the sacrum (S1 is just below L5).
On imaging, L5–S1 is the most discussed level because it is the junction between the mobile lumbar spine and the fixed pelvis.
The sacrum: usually five fused segments
Below L5 is the sacrum, typically made of five fused vertebrae (S1 to S5). It forms the back wall of the pelvis and connects to the hip bones at the sacroiliac joints.
The coccyx: usually 3–5 small fused bones
Below the sacrum is the coccyx (tailbone), commonly 3–5 small segments fused to varying degrees.
Why counting can be tricky
Counting levels is not always as simple as “five lumbar bones, then sacrum.” Some people have an anatomical variation called a lumbosacral transitional vertebra, where the border between lumbar spine and sacrum is blurred. This includes:
- Sacralization (L5 behaves more like part of the sacrum)
- Lumbarization (S1 behaves more like an extra lumbar vertebra)
These variants can change how a radiologist numbers the levels and can matter later if you ever need an injection, procedure, or surgery—because the “level” must be identified correctly.
What happens during a low back pain X-ray
A low back pain X-ray appointment is usually short. The actual image capture often takes only minutes, though positioning can take a bit longer.
What you may be asked to do
- Change into a gown: Metal on clothing can obscure the image (belts, zippers, hooks).
- Remove nearby items: Coins, keys, jewelry, or anything metallic near the abdomen/pelvis.
- Stand or lie down: Depending on the requested views and your comfort.
- Hold your breath briefly: A short breath-hold reduces motion blur.
- Turn slightly for angles: If the team is capturing oblique or spot views.
Common views in a lumbar X-ray series
Radiology practices vary, but a typical low back pain X-ray series may include:
- AP view: A front-to-back image that helps assess overall alignment and side-to-side symmetry.
- Lateral view: A side image that shows the curve (lordosis), disc spaces, and slips more clearly.
- L5–S1 spot view: Sometimes used to better visualize the lowest disc space through the pelvis.
- Oblique views: Less common in routine care now; historically used for pars defects (the “Scotty dog” concept).
- Flexion–extension views: Sometimes requested if instability is suspected; you bend forward and backward to see whether segments translate abnormally.
If your report references “standing” images, that detail can matter because gravity may reveal alignment issues that are less obvious when lying down.
What your report is really doing: describing, not diagnosing
Radiology reports are descriptive summaries of visible anatomy. They are often written to answer a narrow clinical question (for example, “Is there a fracture?” or “Is there a slip?”).
A helpful patient perspective shift:
- The report describes what is visible on a low back pain X-ray.
- Your clinician integrates the report with your symptoms, timeline, and physical exam.
That is why two people with similar “degenerative changes” on a low back pain X-ray can feel very different: the image is not measuring pain.
The most common phrases on a low back pain X-ray report, translated
Below are terms that commonly appear and what they usually mean in plain language.
“No acute osseous abnormality”
This generally means “no new bone problem was seen,” such as no fresh fracture or destructive bone lesion.
It does not mean “no reason for pain exists.”
“Degenerative changes,” “spondylosis,” or “osteoarthritic changes”
These phrases describe wear-and-adaptation patterns at the bony margins and joints—often small bone spurs (osteophytes) and mild joint changes.
These findings are common and tend to increase with age. They can be relevant, but they are not automatically the cause of pain.
“Osteophytes”
Osteophytes are bone spurs. On a low back pain X-ray they may be described as “anterior osteophytes” or “marginal osteophytes.” Many are incidental. Their significance depends on size, location, and whether they plausibly match your symptom pattern.
“Disc space narrowing”
A low back pain X-ray cannot see the disc directly; it sees the space between vertebrae. Narrowing suggests reduced disc height, often from disc dehydration and long-term change.
Disc space narrowing does not confirm a disc herniation and does not measure nerve compression.
“Facet arthropathy”
Facet joints are small joints at the back of the spine that guide movement. “Facet arthropathy” means arthritis-like change in those joints.
On a low back pain X-ray, facet changes can be under-reported because facets are harder to see well than on CT. If this term appears, it generally means the changes were visible enough to comment on.
“Spondylolisthesis,” “anterolisthesis,” or “retrolisthesis”
These terms describe a vertebra slipping forward (anterolisthesis) or backward (retrolisthesis) relative to the one below.
If the report gives a “grade,” it is referring to the degree of slip (Grade 1 is mild). Sometimes the report also mentions whether it appears stable or suggests flexion–extension views.
“Loss of lordosis” or “straightening”
The lumbar spine normally has a gentle inward curve (lordosis). “Straightening” can reflect muscle guarding, positioning during the X-ray, or day-to-day posture.
It is frequently reversible and should not be treated as a permanent structural defect based on wording alone.
“Scoliosis”

Scoliosis is a sideways curve. A report may describe the direction (left or right), location, and sometimes angle. Some curves are structural; others are “functional” and appear during pain episodes or protective muscle tightening.
“Transitional anatomy,” “sacralization,” or “lumbarization”
These terms matter. They describe a variant where the lowest lumbar vertebra (L5) or the top sacral segment (S1) has features of the other region.
If your report mentions transitional anatomy, it is worth ensuring your clinician notes it for future reference.
Sacralization: the missed finding patients should understand
Sacralization is commonly under-explained in routine conversations, yet it can change how your low back pain X-ray is interpreted and how levels are labeled.
What sacralization means
Sacralization is when L5 is partially or completely fused to the sacrum, or when L5 has an enlarged transverse process that forms a joint or fusion with the sacrum or pelvic bone.
In plain terms: the “lowest lumbar bone” behaves more like part of the sacrum.
How it shows up on a low back pain X-ray report
Radiologists may write:
- “Lumbosacral transitional vertebra”
- “Sacralization of L5”
- “Pseudoarticulation of the transverse process”
- “Bertolotti syndrome” (used when the transitional segment is suspected to be pain-related)
Why it matters to you
Sacralization matters for three practical reasons:
- Level numbering can be confusing
With sacralization, what one clinician calls “L5” another might label differently depending on how they count. This matters if someone ever plans an injection, procedure, or surgery. Correct level identification may require additional counting methods or comparison imaging. - Load and motion can shift
When one segment is more fused or behaves differently, motion and load can shift to the level above. That can influence where changes appear on a low back pain X-ray (often above the transitional segment). - It can be linked to symptoms in some people, but not in all
Many people with sacralization have no symptoms. In others, the transitional joint can become irritated and contribute to back or buttock pain. The key point: sacralization is context, not a standalone diagnosis.
Lumbarization: the mirror image
Lumbarization is when the top sacral segment (S1) looks and behaves more like an extra lumbar vertebra. The same cautions apply: numbering can differ, and any relevance must be tied to symptoms.
How radiologists decide what to mention (and what they often do not)
Understanding what drives the report helps you read it more calmly.
Reports prioritize what is reliably visible
Because discs and nerves are not well seen, low back pain X-ray reports tend to emphasize:
- Alignment and curvature
- Bone integrity (fracture vs no fracture)
- Disc space height (indirect)
- Visible joint changes
- Congenital variants (sometimes)
Many “normal variations” are not listed
Reports may not mention small asymmetries or minor variants if they are not considered clinically significant. That can be frustrating, but it is a common reporting practice.
Template language is common
Some reports use structured templates, which can make wording feel generic. The useful part is the specific findings and the impression, not the phrasing style.
Why your symptoms may not match your low back pain X-ray
From a patient perspective, the biggest confusion is mismatch:
- “My X-ray looks bad, but I feel okay.”
- “My X-ray looks normal, but I feel terrible.”
Both are common. Reasons include:
- Pain can come from discs, nerves, muscles, and ligaments—structures that a low back pain X-ray does not show well.
- Some X-ray findings (like mild degenerative changes) are common even in people without pain.
- Pain can be influenced by inflammation and nerve sensitivity, which are physiologic processes not visualized on X-ray.
A practical mindset is: a low back pain X-ray is excellent at ruling in or ruling out certain categories of problems, but it is limited for explaining pain intensity.
X-ray vs MRI vs CT: a patient decision lens
| Test | What it is best at | What it often cannot answer | Typical patient scenario |
|---|---|---|---|
| Low back pain X-ray | Bones, alignment, fractures, transitional anatomy, slips | Disc herniation, nerve compression, most soft tissues | Trauma concerns, suspected instability, baseline alignment questions |
| MRI | Discs, nerves, soft tissue, inflammation | Some bony detail; many incidental findings | Persistent leg symptoms, suspected nerve compression, pre-procedure planning |
| CT | High-detail bone imaging | Higher radiation; less soft tissue detail than MRI | Complex fractures, detailed bony assessment when MRI is not suitable |
Radiation: what patients should know without fear
A low back pain X-ray uses ionizing radiation. In practical terms:
- The risk from a single lumbar series for an adult is generally low.
- The most important safety principle is avoiding unnecessary repeat imaging that will not change decisions.
If pregnancy is possible, inform the imaging center before a low back pain X-ray so appropriate safety protocols can be followed.
Getting the most out of your low back pain X-ray appointment
These patient-centered steps can make the result more useful later:
- Ask whether images are standing or lying down; standing images can better reflect alignment under load.
- If you have prior imaging, ensure it is available for comparison; “no change from prior” can be meaningful.
- Request access to the actual images (portal download or disc) in addition to the report.
- If your report mentions transitional anatomy such as sacralization, keep a note of that for future procedures so level labeling stays consistent.
👨⚕️ Dr. Arora’s Clinical Note:
A common mistake I see is treating the X-ray appointment like a formality and then expecting the report to “explain the pain.” Here’s the practical upgrade that makes imaging more usable: mark the symptom, not just the spine. Before the lateral image, ask the technologist if they can place a small skin marker (they often use a tiny BB-style marker) over your single most painful point (right vs left, near the beltline vs closer to the tailbone). It doesn’t diagnose anything—but it helps your clinician correlate whether the pain behaves more like facet/SI-region irritation vs midline disc-related patterns, especially when the written report is generic.
Counter-intuitive physio tip: if your report says “loss of lordosis/straightening,” don’t rush to aggressive stretching to “restore the curve.” That phrase is often guarding + positioning, and stretching into pain can increase protective spasm. A better first step is 2–3 days of gentle walking + relaxed diaphragmatic breathing + pain-free hip-hinge practice (micro-movements) to downshift the guarding—then reassess.
Red flags: when imaging should not delay urgent evaluation
Seek prompt medical attention if you have:
- New or progressive leg weakness (for example, foot drop)
- Loss of bowel or bladder control, or numbness in the saddle area
- Fever or unexplained chills with severe back pain
- History of cancer with new, persistent back pain
- Severe pain after significant trauma (or minor trauma with high fracture risk)
A low back pain X-ray can be part of evaluation, but these features require clinician assessment regardless of imaging.
What to ask after you receive your report
If you only received a report with no explanation, focus on questions that connect the low back pain X-ray to decisions:
- “Is there any sign of fracture, destructive bone change, or a significant slip?”
- “Do any alignment findings on the low back pain X-ray match my symptom pattern?”
- “Do I have a transitional vertebra such as sacralization, and does it affect level numbering?”
- “Should these X-ray findings be considered stable, or is follow-up imaging ever needed?”
- “If symptoms are mainly leg-related, does MRI add information that the X-ray cannot provide?”
After the midpoint: two reliable references for patients
For a clinician-grade, evidence-based overview of what tends to help (and what usually doesn’t) across acute and chronic low back pain, review: [Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021, 2021].
A report cheat sheet for common findings
| Finding on low back pain X-ray | What it often reflects | Why patients misread it |
|---|---|---|
| Mild spondylosis / degenerative change | Normal wear/adaptation over time | Assumed to equal damage or inevitability |
| Disc space narrowing | Reduced disc height | Assumed to prove herniation or nerve pinch |
| Osteophytes | Bone spurs at margins | Assumed to be “the cause” by themselves |
| Grade 1 anterolisthesis | Mild forward slip | Assumed to require surgery immediately |
| Loss of lordosis | Guarding/positioning | Assumed to be permanent deformity |
| Transitional vertebra / sacralization | Variant anatomy at L5–S1 | Often not explained; can confuse level labeling |
FAQs about low back pain X-ray
1) Does a low back pain X-ray show a disc bulge or herniation?
A low back pain X-ray does not directly show disc bulges or herniations. It may show disc space height changes, but MRI is typically used to visualize discs and nerves.
2) What does “no acute abnormality” mean on a low back pain X-ray?
It usually means no new fracture or destructive bone problem was seen. It does not rule out disc, nerve, or soft-tissue causes of symptoms.
3) If my low back pain X-ray shows degeneration, does that mean my back is “wearing out”?
Degenerative changes on a low back pain X-ray often reflect common, gradual adaptation. They do not automatically predict severe pain or disability.
4) Can a low back pain X-ray diagnose spinal stenosis?
X-ray can show indirect clues (like arthritis or a slip), but it cannot measure spinal canal narrowing well. MRI is typically used to evaluate stenosis.
5) What is sacralization, and why is it mentioned on my report?
Sacralization is a lumbosacral transitional vertebra where L5 partly or fully joins the sacrum. It matters because it can affect level numbering and sometimes shifts load to the level above.
6) What is lumbarization?
Lumbarization is when the top sacral segment behaves more like an extra lumbar vertebra. Like sacralization, it can affect numbering and interpretation.
7) Why did my clinician order an X-ray instead of MRI?
A low back pain X-ray is fast, widely available, and useful for checking bone integrity and alignment. MRI is usually reserved for nerve symptoms, persistent problems, or pre-procedure planning.
8) Should I worry about radiation from a low back pain X-ray?
For most adults, the risk from a single lumbar series is low. The main safety principle is to avoid unnecessary repeat imaging.
9) Can an X-ray miss a fracture?
Yes. Some fractures can be subtle, and visibility depends on views and bone quality. If suspicion is high, clinicians may consider CT or MRI.
10) What should I keep from my imaging visit: the report or the images?
Ideally both. The report is a summary; the images allow comparison over time and can be valuable for second opinions—especially if your low back pain X-ray notes sacralization or other anatomy that affects level labeling.




