If you’re searching for low back pain exercises physical therapy you can do at home, you’re in the right place. The goal of this guide is simple: calm symptoms, move with less fear, and rebuild strength—without guessing, over-stretching, or pushing into a flare.
This is also built to give you more practical value than a random YouTube session. Videos can be useful, but they often miss three things that decide outcomes: (1) how to choose exercises based on your pain pattern or diagnosis, (2) clear “if-this-then-that” safety rules, and (3) a week-by-week progression that tells you exactly what to do next. This article delivers a structured decision tree, diagnosis-informed options, and a progression framework so your low back pain exercises physical therapy is guided, personalized, and progressive from day one.
This low back pain exercises physical therapy program is designed for common, non-emergency low back pain patterns (stiffness after sitting, aches after lifting, “tight” low back, mild referral into the buttock or thigh). It is not a substitute for diagnosis. If you have red flags (listed below), pause the program and seek urgent assessment.
You’ll get:
- A quick self-check to choose the right starting track
- A 7-day “calm it down” reset using low back pain exercises physical therapy
- Disease-wise / diagnosis-informed exercise options (including reduced lumbar lordosis and spinal stenosis)
- A 4-week strength-and-control plan that progresses safely with low back pain exercises physical therapy
- Clear do’s/don’ts, a symptom ruleset, and 10 practical FAQs

Red flags: stop and get checked urgently
Do not continue this low back pain exercises physical therapy plan if you have:
- New bowel or bladder control problems
- Numbness in the groin/saddle area
- Progressive leg weakness, foot drop, or rapidly worsening numbness
- Fever, unexplained weight loss, history of cancer, or recent serious infection
- Significant trauma (fall, accident) or suspected fracture
- Severe pain that is constant, unrelenting, and not position-dependent
If you’re uncertain, get assessed. Safety comes first.
Plain-language glossary (so the rest makes sense)
This low back pain exercises physical therapy guide avoids jargon, but a few everyday terms still help:
- Flare: a temporary spike in pain or symptoms that lasts hours to days. A flare does not always mean damage; it often means your back did more than it could handle that day.
- Muscle guarding: muscles tighten automatically to protect the area. People describe it as “locked,” “stuck,” or “can’t straighten.”
- Spasm: a sudden, strong muscle tightening that feels like a cramp or a “grab.” It can be painful, but it is often a protective response.
- Nerve symptoms: tingling, numbness, burning, or pain that travels down the leg.
- Centralize: leg symptoms move upward (toward the buttock or back) and become less intense. In low back pain exercises physical therapy, that is usually a good sign.
- Irritable back: your back gets angry easily. Small movements, sitting, or bending might trigger it. Irritable backs need smaller exercise doses at first.
- Neutral spine: not forced flat and not forced arched—your comfortable middle.
The one safety ruleset you will use the entire time
These rules apply to every exercise in this low back pain exercises physical therapy program. Because the rules stay the same, you do not have to “relearn” safety every time you change an exercise.
The 24-hour rule
After a session, check symptoms later that day and the next morning:
- Green: discomfort up to 3/10 during exercise and you feel the same or better within 24 hours → continue low back pain exercises physical therapy.
- Yellow: discomfort rises but settles back to your normal level within a few hours → continue but reduce range, reps, or speed in low back pain exercises physical therapy.
- Red: you feel clearly worse the next day, or leg symptoms travel farther down the leg → stop that exercise and switch to another option in low back pain exercises physical therapy.
Stop signs during a rep
Stop the rep or stop the exercise if you feel:
- Sharp, stabbing pain
- A sudden “electric” shock down the leg
- Increasing numbness or weakness
- Dizziness, chest pain, or shortness of breath
How to choose low back pain exercises physical therapy for your pattern or diagnosis
If your back pain were one single problem, one routine would work for everyone. Real life is different. Low back pain exercises physical therapy works best when the exercises match how your symptoms behave.
Step 1: do you have leg symptoms?
Answer yes or no:
- Tingling, numbness, burning, or pain that travels below the knee?
If yes, start with the sciatica/nerve-sensitive track later in this guide. That version of low back pain exercises physical therapy has one special rule: symptoms should move upward (centralize), not spread downward.
Step 2: find your “better direction” (gentle test)
Try each movement for 5 easy reps. You are not testing your limits.
- Bending test: lie on your back and bring one knee toward your chest a little, then return.
- Arching test: lie on your stomach and prop up on elbows a little, then relax.
Which one makes you feel looser or calmer?
- If bending feels better, you’ll likely do well with a flexion-friendly low back pain exercises physical therapy track (often helpful in stenosis).
- If arching feels better, you’ll likely do well with an extension-friendly low back pain exercises physical therapy track (often helpful in some leg-symptom patterns).
- If both feel okay, start with the general track.
Step 3: how reactive is your back today?
If small movements set you off, start with short sessions and the 7-day reset. If you tolerate movement well, you can progress faster within low back pain exercises physical therapy.
Exercise Library: step-by-step instructions (use once, then refer back)
This section is detailed so you do not need a video for technique. Later in the program, when an exercise is listed again, it means “do that exercise using the steps in the library above.” This prevents repetition while keeping low back pain exercises physical therapy easy to follow.
1) 90/90 breathing on a chair

Purpose: reduce protective tension, improve calm breathing, and help you find a comfortable middle position.
How to do it:
- Lie on your back with calves on a chair so hips and knees are bent about 90 degrees.
- One hand on chest, one hand on belly.
- Breathe in through your nose for 3–4 seconds.
- Breathe out through your mouth for 5–6 seconds, slow and controlled.
- Do 6–10 breaths.
Do:
- Keep shoulders relaxed.
- Breathe quietly.
Don’t:
- Hold your breath.
- Force your low back flat.
Stop if:
- You feel dizzy.
2) Pelvic tilt to neutral

Purpose: teach your pelvis and low back to find the “middle,” not stuck flat or stuck arched.
How to do it:
- Lie on your back with knees bent, feet on the floor.
- Gently flatten the low back a little, then gently arch a little.
- Find the middle that feels easiest.
- Repeat slowly for 8–12 reps.
Do:
- Keep motion small.
Don’t:
- Push hard to extremes.
Stop if:
- Sharp pain or worsening leg symptoms.
3) Knee rocks
Purpose: gentle motion for stiffness without forcing a stretch.
How to do it:
- On your back with knees bent, feet on floor.
- Keep knees together and let them fall a few inches to one side.
- Return, then fall to the other side.
- Continue 60–90 seconds.
Do:
- Move like a pendulum.
Don’t:
- Force knees to the floor.
Stop if:
- Pain climbs and stays high afterward.
4) Cat-camel
Purpose: smooth spine motion and control.
How to do it:
- Hands and knees: hands under shoulders, knees under hips.
- Round your back gently (exhale).
- Let your back relax to a mild arch (inhale).
- Do 6–10 slow reps.
Do:
- Keep it smooth.
Don’t:
- Drop into a deep arch if that irritates you.
Stop if:
- Leg symptoms spread downward.
5) Hip hinge rehearsal
Purpose: teach your hips to bend so the low back does not do all the work.
How to do it:
- Stand feet hip-width, knees slightly soft.
- Push hips back as if closing a car door with your butt.
- Keep chest gently lifted, back long.
- Return to standing by squeezing glutes lightly.
- Do 8–12 reps.
Do:
- Move slowly.
Don’t:
- Round your back into a C-shape.
Stop if:
- Sharp pain or worsening leg symptoms.
6) Glute bridge

Purpose: strengthen hips so your back shares load with strong glutes.
How to do it:
- Lie on back, knees bent, feet hip-width.
- Light belly brace.
- Press through heels, lift hips until shoulders-hips-knees form a line.
- Pause 1–2 seconds, lower slowly.
- Do 6–12 reps.
Do:
- Keep it hip-driven.
Don’t:
- Lift so high that the low back pinches.
Stop if:
- Strong hamstring cramps persist (reduce range first).
7) Dead bug (heel taps)
Purpose: core control without crunching or twisting.
How to do it:
- Lie on back, hips/knees at 90 degrees (or keep one foot down).
- Ribs gently down, light belly brace.
- Tap one heel to floor, return.
- Alternate sides for 6–10 reps each side.
Do:
- Move slowly enough to stay controlled.
Don’t:
- Let the low back arch sharply.
Stop if:
- Sharp increase in symptoms.
8) Bird dog
Purpose: coordination between trunk and hips.
How to do it:
- Hands and knees.
- Light belly brace.
- Slide one leg back and straighten; lift slightly if stable.
- Optionally reach opposite arm forward.
- Hold 2 seconds, switch sides, 5–8 reps each.
Do:
- Keep hips level.
Don’t:
- Swing leg high or arch back.
Stop if:
- Sharp pain or spreading leg symptoms.
9) Side plank on knees

Purpose: side trunk strength to stabilize the spine.
How to do it:
- Lie on side, knees bent, forearm under shoulder.
- Lift hips to form a straight line shoulders-hips-knees.
- Hold 15–30 seconds, repeat 2–3 times each side.
Do:
- Keep shoulder away from ear.
Don’t:
- Let hips roll backward.
Stop if:
- Sharp shoulder pain or symptom spike.
10) Supported split squat

Purpose: leg strength with a stable trunk.
How to do it:
- Stand near a wall or chair for support.
- Step one foot back into a split stance.
- Lower a few inches by bending both knees.
- Push through the front foot to rise.
- Do 6–10 reps each side.
Do:
- Start with small range.
Don’t:
- Let the front knee collapse inward.
Stop if:
- Back pain spikes; reduce range or switch to sit-to-stand.
11) Sit-to-stand
Purpose: strength for daily tasks.
How to do it:
- Sit tall on a chair, feet under knees.
- Lean slightly forward from hips (use hip hinge feel).
- Stand, then sit down slowly with control.
- Do 6–12 reps.
Do:
- Use hands lightly if needed.
Don’t:
- Drop back into the chair.
Stop if:
- Sharp pain or dizziness.
12) Suitcase carry
Purpose: train real-life stability.
How to do it:
- Hold a light weight or bag in one hand.
- Stand tall, ribs over pelvis.
- Walk 20–40 steps, switch hands, repeat.
Do:
- Keep shoulders level.
Don’t:
- Lean into the weight.
Stop if:
- Sharp increase in symptoms.
Disease-wise tracks: pick the set that fits you
If you already know your diagnosis, use the matching low back pain exercises physical therapy track. If you do not know, choose the track that makes you feel calmer after a short trial.
Track A: reduced lumbar curve (loss of lordosis / “flat back feel”)
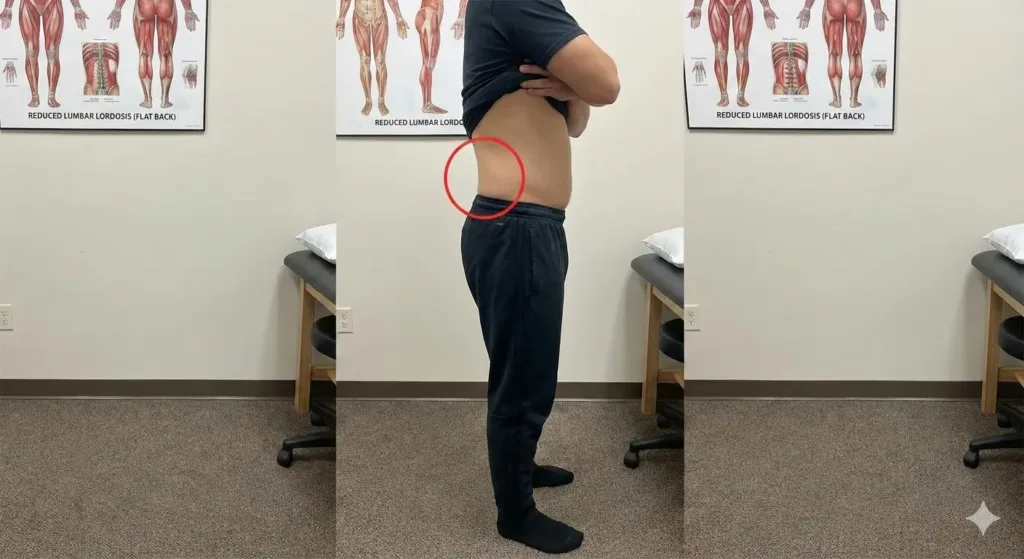
What it can feel like:
- Low back feels flat and tired after sitting
- Standing feels uncomfortable
- Hips feel stiff; hamstrings feel tight
Choose these from the Exercise Library:
- 90/90 breathing on a chair
- Pelvic tilt to neutral
- Hip hinge rehearsal
- Glute bridge
- Dead bug
- Sit-to-stand
Limit for now:
- Long slumped sitting without breaks
- Aggressive toe-touch stretching if it flares you
Why this track helps:
It restores movement variety and hip strength so the low back is not the only place that bends and works.
👨⚕️ Dr. Arora’s Clinical Note:
Many patients ask me if stretching is the “missing piece” for low back pain. Here’s the counter-intuitive truth: a lot of what feels like tightness is actually protective guarding, not a true muscle shortness problem. If you stretch guarding, you often teach the nervous system that the area is “unsafe,” and symptoms can linger or flare.
A simple clinical shortcut: if a stretch gives a sharp, nervy, or “electric” feel (or makes leg symptoms travel farther), don’t stretch it yet. Instead, use isometrics to calm the system and recruit support muscles without provoking the back. Try this for 3–5 days:
- Bridge hold (small range): lift only until comfortable, hold 10 seconds × 5 reps, rest 20–30 seconds.
- Wall sit (shallow): hold 15–25 seconds × 3, keep ribs over pelvis.
- Then re-test a gentle stretch: if it feels easier (not sharper), you’ve “earned” stretching back safely.
Track B: lumbar spinal stenosis (often prefers bending-forward positions)
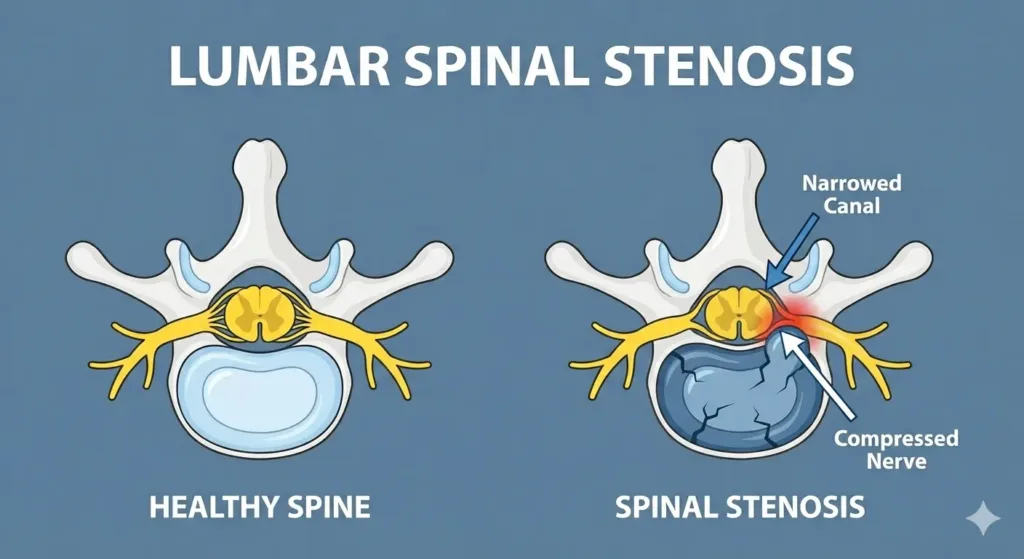
What it can feel like:
- Leg heaviness, cramping, numbness, or pain when standing or walking
- Relief when sitting, bending forward, or leaning on a cart
Choose these from the Exercise Library:
- 90/90 breathing on a chair
- Pelvic tilt to neutral
- Knee rocks
- Dead bug
- Glute bridge (small range)
- Suitcase carry (light)
Walking rule for this track:
Use intervals: walk 2–6 minutes, sit 1–2 minutes, repeat.
Limit for now:
- Long standing in a big arch posture
- Long downhill walks if they worsen symptoms
Track C: sciatica or nerve-sensitive leg symptoms
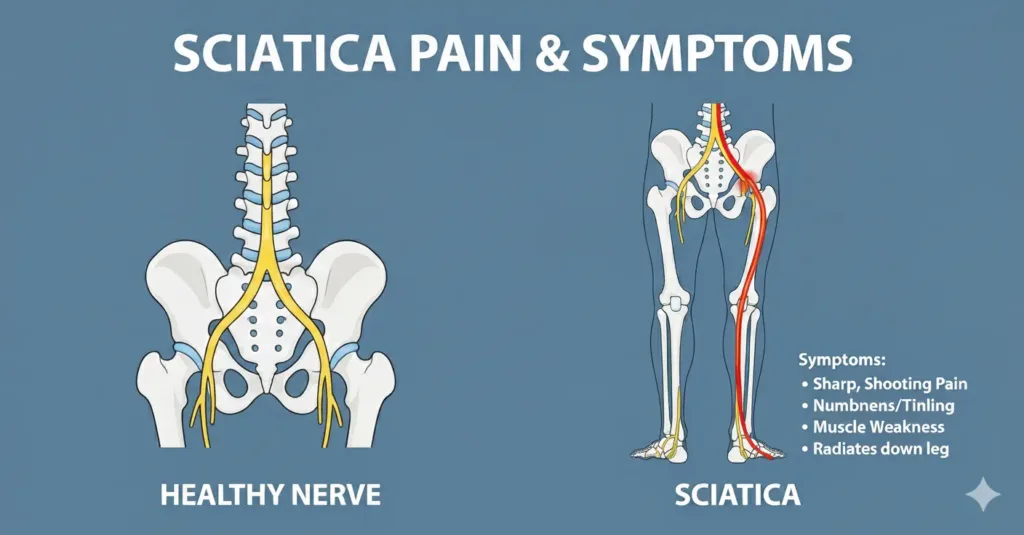
What it can feel like:
- Tingling, numbness, burning, or pain that travels down the leg
- Sitting, bending, or standing changes symptoms quickly
Use these from the Exercise Library:
- 90/90 breathing on a chair
- Pelvic tilt to neutral
- Knee rocks
- Dead bug (use the easier version if needed)
- Suitcase carry (very light, only if tolerated)
Then add a direction bias (do not guess; test it):
- If arching helps and leg symptoms move upward, add the prone-on-elbows drill in the “Nerve Symptoms Add-On” section.
- If bending helps and symptoms calm, add the single knee-to-chest drill in the “Nerve Symptoms Add-On” section.
Limit for now:
- Stretching into leg pain
- Long sitting without breaks
Track D: extension-sensitive back (often facet irritation or spondylolisthesis patterns)
What it can feel like:
- Pain worse with arching backward or standing too long
- Pain with twisting plus arching
Choose these from the Exercise Library:
- 90/90 breathing on a chair
- Pelvic tilt to neutral
- Dead bug
- Bird dog
- Side plank on knees
- Supported split squat
- Suitcase carry
Limit for now:
- Deep backbends or repeated arching drills
The Calm-Down Reset (Days 1–7)
This is the first phase of low back pain exercises physical therapy for most people. It lowers irritability and builds confidence before heavier work.
Daily plan (10–15 minutes):
- Downshift: 90/90 breathing on a chair (see Exercise Library)
- Gentle motion: knee rocks or cat-camel (see Exercise Library)
- Control + strength: pick 2 exercises from your track (use the library steps)
- Optional short walk: 5–12 minutes if it helps
If you wake up stiff:
Do a mini-session in the morning and another later. Two small doses often work better than one big session in low back pain exercises physical therapy.
If you feel “locked up”:
Use smaller ranges. Your goal is to feel even 10–20% easier after the session.
The 4-week low back pain exercises physical therapy home program
This is the capacity phase: you strengthen hips, legs, and trunk so everyday tasks stop re-triggering symptoms.
Progress rules (choose one change only):
- Add 1–2 reps
- Add 5 seconds to holds
- Add a small load (backpack, band)
- Slow the lowering phase
Weekly schedule:
- Day 1: Strength A
- Day 2: Mobility + walking
- Day 3: Strength B
- Day 4: Mobility + walking
Optional: short easy walk on other days
Warm-up (5 minutes):
- 90/90 breathing on a chair
- Cat-camel or knee rocks
- Hip hinge rehearsal
(See the Exercise Library for how to do each.)
Week 1: confidence and control
This week of low back pain exercises physical therapy is about feeling safer with movement and finishing sessions feeling steadier.
Strength A:
- Choose 4 items: one hip strength (bridge), one core control (dead bug), one stability (side plank or bird dog), and one carry.
- Do 3 sets for the first three items; do 4 carry walks.
Strength B:
- Choose 4 items: one stability (bird dog or side plank), one leg strength (split squat or sit-to-stand), one hinge practice, and one carry.
Walking day guidance:
- If walking helps, do 10–20 minutes total.
- If you are on the stenosis track, use walking intervals.
Week 2: build endurance
In low back pain exercises physical therapy, Week 2 is where you prove to your back that you can repeat work without a rebound flare.
Keep the same exercise list and progress only one variable. The biggest mistake in low back pain exercises physical therapy is changing exercises too often; consistency beats novelty.
Add two movement breaks daily:
Every 30–45 minutes of sitting:
- Stand and do 6 hip hinges OR walk for 60 seconds.
Week 3: strengthen the hinge and legs
This is the phase where low back pain exercises physical therapy starts translating into easier lifting, stairs, and longer days.
Strength A:
- Glute bridge: 3×10 (or add a 2-second pause)
- Dead bug: 3×8 each side
- Sit-to-stand: 3×10 (slow down on the way down)
- Side plank: 3×20–40 seconds
Strength B:
- Hip hinge rehearsal: 3×10 (add a backpack only if Week 2 was stable)
- Supported split squat: 3×8 each side
- Bird dog: 3×6 each side with a 2-second pause
- Suitcase carry: 4×30–40 steps
Week 4: return-to-life capacity
Think of Week 4 low back pain exercises physical therapy as “practice for real life”: carry, stand, walk, and bend with fewer consequences.
Strength A:
- Hip hinge with light load (backpack): 3×8
- Supported split squat: 3×8 each side
- Suitcase carry: 4×40 steps
- Dead bug: 2×8 each side
Strength B:
- Sit-to-stand: 3×12
- Stair practice: 2–3 minutes with breaks (if tolerated)
- Side plank: 3×30–45 seconds
- Bird dog: 2×8 each side
Nerve Symptoms Add-On (only if you have leg pain/tingling)
For nerve symptoms, low back pain exercises physical therapy must follow one priority: symptoms should not spread farther down the leg.
Choose ONE direction add-on, based on your gentle direction test:
If bending helps:
- Single knee-to-chest: 6 reps each side, small range, then stop.
If arching helps:
- Prone on elbows drill:
- Lie on stomach.
- Prop on elbows for 10–20 seconds.
- Relax for 20 seconds.
- Repeat 4–6 times.
Use the 24-hour rule. If symptoms spread farther, stop that add-on and switch.
Daily-life habits that make the plan work faster
These habits are not extra homework; they are the “multiplier” that helps low back pain exercises physical therapy work with less effort.
Low back pain exercises physical therapy works better when you stop feeding the same trigger all day.
Sitting plan (simple)
- Change position every 30–45 minutes.
- Use a small rolled towel at the low back if it feels better.
- Do not chase “perfect posture.” Aim for “comfortable, changeable posture.”
Lifting plan (simple)
- Use the hip hinge feel you practiced.
- Hold objects close to your body.
- Exhale gently during effort.
Sleep comfort (simple)
- Side sleeper: pillow between knees.
- Back sleeper: pillow under knees.
Small comfort changes can reduce overnight guarding so low back pain exercises physical therapy feels easier the next morning.
After you have a plan, it can be useful to read a general medical overview for warning signs and common causes:
After you have a plan, cross-check it against evidence-based physiotherapy guidelines and high-quality reviews used in clinical practice: [Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021, 2021]
FAQs
1) How many exercises should I do per day?
Most people do best with 4–6 exercises total. A smaller set done consistently usually beats doing 12 different moves once.
2) How long should a session take?
During Week 1, 10–15 minutes is enough. Later, 20–30 minutes on strength days is typical.
3) Should I stretch daily?
Stretching can help if it makes you feel better and does not flare symptoms. Many people improve more from strength and control than from aggressive stretching.
4) Is walking always good?
Walking often helps, but dose matters. If walking flares you, use shorter intervals with breaks and build gradually.
5) If I have spinal stenosis, is bending forward “bad posture”?
Not necessarily. Many stenosis patterns feel better with a slight forward lean. The goal is function and symptom control.
6) If I have loss of lordosis, should I force an arch?
No. Forcing an arch can irritate some backs. Build neutral control and hip strength instead.
7) What if I feel pain during an exercise but better afterward?
That can happen. Use the 24-hour rule. If you are not worse the next day, it is usually fine to continue with small adjustments.
8) When can I return to gym lifting?
When daily activities are improving and you can hinge and sit-to-stand without a next-day flare. Start lighter, fewer sets, and progress slowly.
9) Why do hamstrings cramp during bridges?
Often the glutes are not contributing enough. Reduce range, focus on pressing through heels, and build gradually.
10) What is the fastest way to prevent flares from returning?
Build baseline capacity: hips, legs, carries, walking, and frequent position changes. That combination is what makes low back pain exercises physical therapy durable.




