If you notice low back pain before period almost like clockwork—one to three days before bleeding starts—you are not imagining it. This pattern is common, and for many people it is driven more by hormone and uterus-related changes than by “a bad back.” At the same time, low back pain before period is not one single condition. It can be a mix of menstrual cramps, pelvic pressure, fluid retention, sleep disruption, stress, and ordinary muscle overload that just feels louder in the premenstrual window.
This guide explains why low back pain before period happens, what it tends to feel like, and what actually helps at home—step by step—without scary language or vague advice. You will also learn the red flags that mean your symptoms deserve a medical evaluation.

What premenstrual low back pain typically feels like (and why it varies)
Premenstrual low back pain can show up as:
- A dull ache across the beltline, sometimes spreading into the buttocks.
- A deep “pressure” sensation that feels inside the pelvis rather than on the surface muscles.
- Tightness or stiffness when you stand up after sitting.
- A crampy ache that comes in waves (often tied to uterine contractions).
- A flare of an old back issue (disc, facet, SI joint) that feels worse than usual.
Two people can have the same cycle timing and totally different sensations. The difference often comes from:
- Where the pain is generated (uterus/pelvis vs. muscles/joints).
- How sensitive your nervous system is that week (sleep, stress, workload).
- How much bloating or fluid retention is present.
- Your baseline movement habits (long sitting, lots of bending, heavy lifting).
A useful clue is timing: pain that peaks right before bleeding and improves within the first 1–3 days of flow is more likely hormonally and prostaglandin-driven. Pain that is unrelated to the cycle, progressively worsening, or triggered clearly by a movement pattern may be more mechanical.
The biology behind low back pain before period
Understanding the “why” makes the “what helps” much more predictable.
1) Prostaglandins: the cramp chemicals that can refer pain to the back
In the days leading up to bleeding, the uterine lining releases chemicals called prostaglandins. Prostaglandins help the uterus contract so it can shed its lining. Stronger contractions can create pelvic pain that your brain interprets as back pain because the uterus and the lower back share some nerve pathways. That is why a uterus-driven issue can feel like it sits right over your sacrum.
Clues that prostaglandins are a big driver:
- Crampy waves, sometimes with nausea or loose stools.
- Pain that improves once bleeding is established.
- A “deep” ache that is hard to point to with one finger.
2) Hormone shifts change pain sensitivity and joint “tolerance”
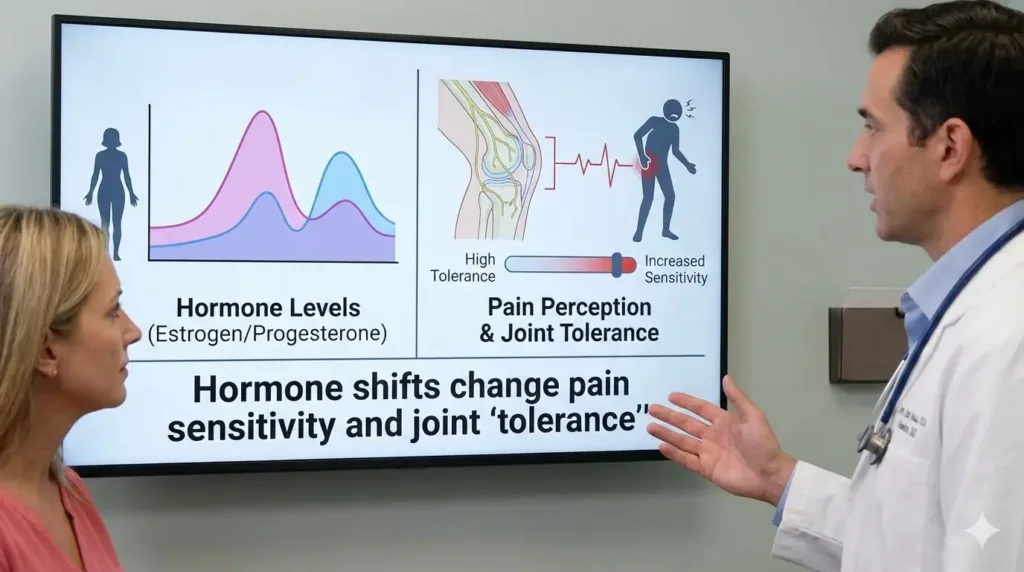
The late luteal phase (the days before bleeding) involves shifts in progesterone and estrogen. These shifts can:
- Change how your nervous system processes discomfort (a lower threshold can make normal loads feel painful).
- Increase perceived stiffness.
- Influence ligament and joint “give,” which may make the pelvis and low back feel less stable in people who already have SI joint or lumbar irritation.
This does not mean your joints are “loose” in a dangerous way. It means your system may need a little more support—better sleep, steadier movement, and fewer high-strain positions—during the window when symptoms tend to appear.
3) Fluid retention and bloating alter pressure and posture
Many people retain fluid premenstrually. Bloating can change abdominal pressure and breathing patterns, which can shift how your trunk muscles support the spine. When the belly feels distended, it is common to arch the low back slightly more or brace awkwardly, both of which can amplify discomfort.
4) Stress, poor sleep, and fatigue “turn up the volume”
Premenstrual insomnia, anxiety, or irritability can make pain feel sharper. Stress also increases protective muscle guarding—your muscles tighten to “protect” you—which can make the low back feel locked. If your week is already busy, a premenstrual flare can be the final straw rather than the only cause.
Common causes and contributors (beyond “just cramps”)
Use this as a menu of possibilities. More than one can be true.
Very common and usually benign contributors
- Primary dysmenorrhea (period cramps without an underlying disease)
- Referred pain from uterine contractions (prostaglandins)
- Premenstrual bloating and fluid retention
- Constipation or gas pressure (often worse premenstrually)
- Reduced activity + more sitting (fatigue week)
- Muscle overload from normal life (lifting, cleaning, workouts)
- Hip flexor tightness from prolonged sitting
- Glute fatigue and pelvic control changes
- SI joint irritation (especially with asymmetrical loads)
- Lumbar facet joint irritation (arch-heavy postures)
- Old injury sensitization (a prior back episode flares)
- Sleep deprivation and stress-related muscle guarding
Less common, but important to consider if symptoms are severe or changing
- Endometriosis (often pain before and during bleeding; may include pain with sex or bowel movements)
- Adenomyosis (often heavy bleeding and cramping; deep pelvic ache)
- Fibroids (pressure, heavy periods, urinary frequency)
- Pelvic inflammatory disease or infection (pain + fever/discharge)
- Ovarian cyst irritation or torsion risk (sudden, one-sided, severe pain)
- Urinary tract infection (burning urination, fever, flank pain)
- Kidney stone (sharp waves, blood in urine)
- Early pregnancy issues (if pregnancy is possible)
- Non-cycle mechanical back conditions (disc, stenosis, spondylolisthesis)
A quick comparison table
| Pattern | More likely | What usually helps first |
|---|---|---|
| Crampy waves, deep pelvic ache that feels premenstrual | Prostaglandins / dysmenorrhea | Heat, gentle movement, anti-inflammatory strategies |
| Stiff after sitting, better after walking | Muscle guarding, joint irritation | Walking breaks, hip mobility, supported positions |
| One-sided sharp pain, sudden onset | Cyst irritation, kidney/urinary causes | Medical assessment, avoid self-treating |
| Pain with fever, unusual discharge, or burning urination | Infection | Medical assessment promptly |
| Pain linked to bending/lifting pattern, not strictly cycle-timed | Mechanical back source | Technique changes, graded strengthening |
Quick self-check: is your pain likely cycle-related?
Ask these questions:
- Does the pain start within 7 days before bleeding and ease within the first 1–3 days?
- Is it paired with other PMS signs (bloating, breast tenderness, mood shift)?
- Does heat help more than stretching?
- Does gentle walking feel better than complete rest?
If most answers are “yes,” it is reasonable to treat it as cycle-influenced first. If low back pain before period is new, severe, one-sided, or comes with red flags (listed later), skip home management and get checked.
What actually helps: a practical relief plan (48 hours to day 1)
The goal is not to “fix everything in one day.” The goal is to reduce pain signals, improve comfort, and prevent the pain from snowballing.
Step 1: De-threaten the area (first 10–20 minutes)
A. Heat (simple and effective)
Use a heating pad or hot water bottle over the lower abdomen or low back for 15–20 minutes. Heat can reduce cramp intensity and relax guarding muscles, which is why it often helps quickly.
Do:
- Keep the heat warm, not scalding.
- Use a thin layer of clothing between heat and skin.
Don’t: - Fall asleep on high heat.
- Use heat on areas with numbness or impaired sensation.
B. Two positions that “unload” the low back and pelvis
Pick one and stay 3–5 minutes while breathing slowly.
1) 90/90 supported rest
- Lie on your back near a sofa/bed.
- Place lower legs on the seat so hips and knees are both about 90 degrees.
- Let your low back soften; do not force it flat.
- Breathe in through the nose for 4 seconds, out for 6 seconds, for 6–10 breaths.
2) Side-lying pillow support

- Lie on your side with a pillow between the knees.
- Add a small rolled towel under the waist if you feel a gap.
- Keep shoulders relaxed, jaw unclenched, slow breathing.
These are not exercises; they are nervous-system “downshifts” that make the whole flare easier to manage.
Step 2: Gentle movement “snacks” (repeat 2–4 times/day)
Total rest often worsens stiffness. Use small, non-scary movements.
A. 5-minute walk
Walk at a comfortable pace for 5 minutes. If it helps, repeat later. This is one of the highest-return strategies for low back pain before period because it improves circulation and reduces guarding.
B. Pelvic tilts (pain-free range)
- Lie on your back with knees bent, feet flat.
- Imagine your pelvis is a bowl of water.
- Gently tip the bowl toward your face (flatten slightly) and then away (small arch).
- 8–12 slow reps, no breath-holding.
Do:
- Keep the movement small and smooth.
Don’t: - Push into sharp pain.
- Turn it into a hard core workout.
Step 3: Targeted mobility (choose 2; total 6–8 minutes)
These are designed to address common premenstrual contributors (hip flexor tightness, glute stiffness, lumbar sensitivity) without aggressive stretching.
Option 1: Hip flexor “couch” stretch (gentle version)
- Kneel with one knee on a cushion near a wall or sofa.
- Place the other foot forward so you are in a lunge stance.
- Tuck the tail slightly (think “zip up” the lower belly) to avoid over-arching.
- Shift forward until you feel a mild stretch at the front of the hip.
- Hold 20–30 seconds, 2 times each side.
Stop if:
- You feel pinching in the front of the hip.
- Symptoms spike sharply (reduce the stretch or switch options).
Option 2: Figure-4 glute stretch (supported)
- Lie on your back, knees bent.
- Cross ankle over opposite knee (a “4” shape).
- Hold behind the thigh of the bottom leg and gently bring it toward you.
- Hold 20–30 seconds, 2 times each side.
Option 3: Child’s pose with side reach (for back tightness)
- Kneel, sit hips back toward heels.
- Reach arms forward; then walk hands slightly to the right to stretch the left side.
- 3–4 slow breaths, then switch.
If child’s pose bothers your knees or hips, skip it.
Step 4: Stabilize without strain (3 simple strength moves)
Strength work is not about “six-pack abs.” It is about giving the spine and pelvis steady support so low back pain before period does not spiral.
Move 1: Glute bridge (easy version)
- Lie on your back, knees bent, feet hip-width.
- Exhale gently and squeeze glutes to lift hips a few inches.
- Pause 2 seconds, lower slowly.
- 8–10 reps, 1–2 sets.
Do:
- Keep ribs relaxed (no big arch).
Don’t: - Push through hamstring cramps (place feet slightly closer to butt, or reduce lift).
Move 2: Side plank on knees (beginner-friendly)
- Lie on your side, knees bent, elbow under shoulder.
- Lift hips so your body forms a straight line from shoulders to knees.
- Hold 10–20 seconds, 2–3 times each side.
Stop if:
- Shoulder pain or sharp side pain appears.
- Your back pain worsens during the hold.
Move 3: Dead bug “march” (tiny range)
- Lie on your back, knees bent at 90 degrees (tabletop) if comfortable; otherwise keep feet on floor.
- Brace lightly as if preparing for a cough.
- Slowly lower one heel to tap the floor, return, then switch.
- 6–10 taps each side.
This is a control exercise, not a speed drill.
Step 5: Smart daily habits that make a real difference
Hydration + steady meals
Skipping meals can increase fatigue and irritability, which increases pain sensitivity. Aim for regular meals and hydration; it supports energy and reduces the “wired-tired” feeling that can worsen low back pain before period.
Magnesium and supplements (caution)
Some people try magnesium for cramps. If you use supplements, check with a clinician, especially if you have kidney issues or take medications. Do not assume “natural” equals “risk-free.”
Over-the-counter pain relief (use safely)
Anti-inflammatory medicines can help prostaglandin-driven cramps for some people, but they are not suitable for everyone (stomach ulcers, kidney disease, blood thinners, certain asthma, pregnancy, etc.). If you are unsure, consult a pharmacist or clinician. This article cannot replace personalized medical advice.
👨⚕️ Dr. Arora’s Clinical Note:
A common mistake I see is treating premenstrual back pain like a pure “tight back” problem—and then stretching hard or repeatedly bending forward to chase relief. When the timing is clockwork (1–3 days before bleeding), the low back is often reacting to pelvic pressure, bloating-driven posture changes, and a more sensitive nervous system.
Physio secret: don’t try to “win” with flexibility—change pressure and position first. Try this 3-minute reset during a flare:
- 90/90 breathing for 6 slow breaths (inhale 4 sec, exhale 6–8 sec), letting the ribs soften down.
- On the last exhale, add 5 gentle pelvic tilts (tiny range).
- Stand and do a 2-minute easy walk.
If you’re someone whose cramps are predictable, the counter-intuitive tip is timing: starting your best strategy early (before it peaks) usually beats “waiting until it’s unbearable.” If any stretch gives a sharp pinch in the front of the hip or increases your back arch, make it milder—or skip it that day.
A 7-day reset plan if low back pain before period keeps returning
If low back pain before period returns most cycles, treat the week before bleeding as a predictable training block rather than a surprise.
Days -7 to -4: Build a buffer
- Walk 15–25 minutes most days.
- Do the 3 strength moves above on 2 non-consecutive days.
- Add one mobility option after sitting-heavy days.
Days -3 to -1: Lower the load, increase the support
- Reduce high-strain workouts (max lifts, deep backbends, long runs) if they reliably trigger a flare.
- Use heat once daily.
- Keep movement snacks: 5-minute walks, pelvic tilts.
- Prioritize sleep routines (consistent bedtime, less late caffeine).
Day 0 to Day 2: Comfort-first
- Pick two interventions that reliably work for you (often heat + walking).
- Use supported rest positions when symptoms peak.
- Keep mobility gentle; avoid “stretching hard to make it go away.”
When premenstrual low back pain is a sign of something more
Most cases are manageable. Some are not. Seek medical care urgently if you have:
- Sudden severe pain (especially one-sided) that is new.
- Fever, chills, or feeling acutely unwell.
- Fainting, dizziness, or severe weakness.
- Heavy bleeding (soaking pads/tampons very quickly), or bleeding between periods.
- New pain with sex, bowel movements, or urination.
- Possible pregnancy, missed period, or positive test with pain.
- Numbness in the groin/saddle area, or loss of bowel/bladder control.
- Back pain that is constant, progressive, or unrelated to your cycle.
If you have recurring low back pain before period with deep pelvic pain, pain during sex, or bowel/bladder symptoms, ask specifically about conditions like endometriosis or adenomyosis. Getting the right label matters because the “best next step” changes.
How clinicians evaluate recurring low back pain before period
A good evaluation usually includes:
- A symptom timeline (when it starts, peaks, resolves).
- Bleeding pattern (heavy, clots, spotting).
- Associated symptoms (GI, urinary, pain with sex).
- Movement triggers (bending, sitting, lifting).
- A pelvic exam when appropriate.
- Sometimes ultrasound or lab work, depending on symptoms.
Imaging of the spine is not always needed for low back pain before period. If the pattern is strongly cycle-tied and you have no neurological symptoms, pelvic causes may be more relevant. If the pain is mechanical and persists beyond the cycle, spine-focused assessment may be useful.
Evidence-based references you can trust
For a research-based overview of dysmenorrhea (period pain) treatments and what the evidence says about anti-inflammatory options, see: [Nonsteroidal anti-inflammatory drugs for dysmenorrhoea, 2015].
Prevention stack: how to reduce low back pain before period over time
Think of prevention as a stack, not a single magic fix.
1) Build “hip and trunk capacity”

Two to three days per week, keep a simple routine:
- Glute bridge or hip hinge pattern
- Side plank on knees progressing to full side plank
- Dead bug variations
- Squat-to-chair (pain-free range)
More capacity means the same daily loads are less likely to trigger low back pain before period.
2) Manage sitting like a professional
Long sitting is a common amplifier.
- Stand up every 30–45 minutes for 60–90 seconds.
- Do 6 pelvic tilts or a short walk.
- Avoid perching on the edge of the chair with an exaggerated arch.
3) Reduce asymmetrical loading in the premenstrual window
In the days when low back pain before period usually hits:
- Switch sides when carrying bags.
- Avoid one-hip standing for long durations.
- Use a step stool when doing sink tasks (one foot on stool reduces lumbar strain).
4) Consider pelvic floor contribution (without panic)
The pelvic floor is a sling of muscles inside the pelvis that helps manage pressure. Some people develop pelvic floor over-tension in stress-heavy weeks; others have weakness and poor coordination. Clues include pelvic heaviness, urinary urgency, pain with penetration, or pain that feels “deep.” If these exist with low back pain before period, a clinician trained in pelvic health can assess whether down-training or strengthening is appropriate.
Myth vs. fact
| Myth | Fact |
|---|---|
| “Low back pain before period means something is wrong with my spine.” | More often, that back ache is being driven by premenstrual hormone shifts and uterus/pelvic activity, which can temporarily make the area feel more sensitive—without any new spinal damage. |
| “If stretching doesn’t help, nothing will.” | Heat, walking, supported rest, and gentle stabilization can help even when stretching fails. |
| “I should rest completely until it passes.” | Staying still for long stretches can make your back tighten up even more. Short, easy bouts of movement—like a few minutes of walking or gentle mobility—often reduce the ache faster than complete rest. |
| “Pain is normal, so I should ignore it.” | Mild discomfort can be common; severe, changing, or disabling pain deserves evaluation. |
FAQs about low back pain before period
1) How many days before bleeding can low back pain before period start?
Low back pain before period can start anywhere from a few hours to about a week before bleeding, but many people notice it most strongly 1–3 days beforehand. A consistent pattern that eases once bleeding starts is a common clue that prostaglandins and hormone shifts are involved.
2) Can low back pain before period be the only symptom of PMS?
Yes. Some people have very little mood change or bloating but still report low back pain before period as their main premenstrual symptom. That said, if the pain is new, severe, or progressively worsening, consider an evaluation to rule out non-PMS causes.
3) Why does low back pain before period feel worse when I sit?
Sitting increases load on the lumbar discs and can shorten hip flexors. In the premenstrual window, tissues may be more sensitive, so the same sitting posture feels worse. Try brief standing breaks, a short walk, or the 90/90 supported rest position.
4) Is premenstrual back pain related to constipation?
It can be. Constipation and gas can increase pelvic pressure and make cramps feel stronger, which can present as low back pain before period for some people. Hydration, gentle walking, and fiber-rich meals often help, but persistent constipation should be discussed with a clinician.
5) Could low back pain before period be endometriosis?
It could, especially if pain starts before bleeding and continues through the period, or if you also have pain with sex, bowel movements, or significant fatigue. Low back pain before period alone does not confirm endometriosis, but recurring deep pelvic pain is a reason to get assessed.
6) Does exercise help or worsen symptoms?
It depends on intensity. Gentle movement and light strength work often help low back pain before period, while high-intensity workouts that involve heavy lifting or deep backbends may worsen symptoms for some. Use the “talk test” and keep effort moderate during flare days.
7) What is the fastest home approach for low back pain before period?
For many people, the fastest combination is heat (15–20 minutes) plus a short walk. If you need additional relief, add a supported rest position and gentle pelvic tilts. The best option is the one you can repeat safely.
8) When should I worry about low back pain before period?
Worry less about mild, predictable discomfort and more about changes: sudden severe pain, one-sided sharp pain, fever, heavy bleeding, fainting, or possible pregnancy. Low back pain before period with neurological signs (numbness, weakness, bowel/bladder changes) also needs urgent attention.
9) Can low back pain before period happen with a normal ultrasound?
Yes. Primary dysmenorrhea and prostaglandin-driven pain can occur even when scans are normal. A normal ultrasound does not mean low back pain before period is “in your head”; it often means there is no structural pelvic mass, which is still useful information.
10) How can I reduce low back pain before period next month?
Track your pattern for one cycle, then use a prevention stack: consistent walking, two weekly strength sessions, sitting breaks, and reduced asymmetrical loading in the 3 days before symptoms usually start. Many people find that treating low back pain before period proactively works better than reacting at the peak.




