“Expert Review: This article includes clinical insights from Dr. Arora, a physiotherapist with 20 years of experience.”
Feeling low back pain and stomach pain at the same time can be unsettling—especially when it hits out of nowhere or keeps coming back. People often assume it must be “something in the spine,” or they panic that it’s “something in the belly.” If you’re noticing low back pain with bloating, that detail can be especially helpful for narrowing the likely lane (bowel vs. urinary vs. pelvic).
In reality, low back pain and stomach pain can travel together for a few different reasons: sometimes it’s a true abdominal or pelvic condition that refers pain to the back, sometimes it’s a back problem that “feels” like abdominal discomfort, and sometimes you simply have two issues happening at once (for example, constipation plus a back strain). The key is to use symptom patterns—timing, triggers, and “extra” clues like fever, urinary changes, or menstrual timing—to decide what needs urgent care and what can be managed conservatively.
This guide is designed to help you think like a clinician, without medical jargon. You’ll learn why low back pain and stomach pain can share the same wiring, the red flags that require urgent evaluation, and the 7 most important causes doctors watch for—ranging from very common (kidney stones, urinary infections) to rare but dangerous (abdominal aortic aneurysm). You’ll also get a practical “what to do next” plan and a gentle rehab approach if serious causes have been ruled out.
Educational note: This article is for education only and does not replace an in-person medical exam. If your symptoms are severe, sudden, or accompanied by red flags, seek urgent care.

Low back pain and stomach pain: why they can show up together
When low back pain and stomach pain happen together, the “why” is often about shared nerve pathways and shared real estate in the trunk.
1) Referred pain: one problem, two locations
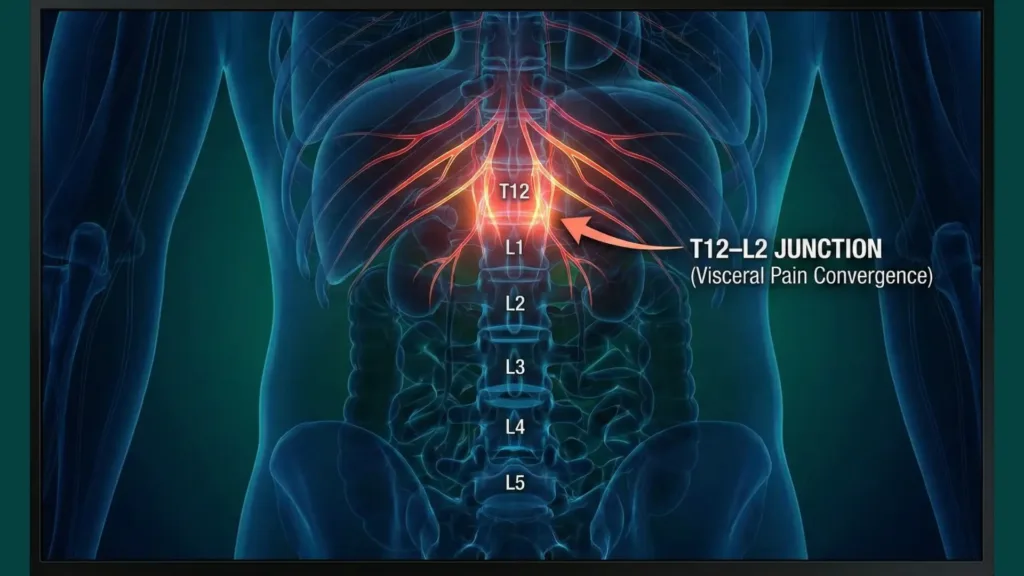
Organs in your abdomen and pelvis send pain signals to the spinal cord. Those signals enter at specific spinal levels (segments). Your brain is much better at locating pain from skin and muscles than pain from internal organs, so it sometimes “maps” internal pain to nearby body regions—commonly the back, flank, groin, or lower abdomen. This is why kidney and bowel problems can feel like low back pain and stomach pain at the same time.
2) Shared muscles and fascia: the “core can transmit pain” effect
The front of the abdomen, the sides of the trunk, and the low back share a continuous fascial system (think: a strong sheet of connective tissue). If you have a strong cough, vomiting, lifting strain, or a sudden twist, you can irritate both abdominal wall tissues and lumbar tissues. The result can be lower back and abdominal pain that feels “linked,” even though no organ disease is present.
3) The “two problems at once” scenario is common
It is surprisingly common to see low back pain and stomach pain together because of two overlapping, treatable issues—such as constipation plus a lumbar strain, or a urinary infection plus back muscle guarding. This is why pattern recognition (what it feels like, what triggers it, and what other symptoms travel with it) matters more than guessing.
Red flags: when low back pain and stomach pain is an emergency
If you have low back pain and stomach pain with any of the red flags below, do not try to “stretch it out” or wait it out—get urgent medical evaluation (ER / A&E). In the US call 911; in the UK call 999; in Canada call 911.
Seek urgent care now if you have:
- Sudden, severe abdominal pain with fainting, dizziness, clammy skin, or very low blood pressure
- Severe back pain plus a “ripping/tearing” abdominal sensation
- Fever (especially with chills) plus flank/back pain, or you feel very unwell
- Persistent vomiting, inability to keep fluids down, or signs of dehydration
- Blood in urine or painful urination with systemic symptoms
- Black, tarry stools or vomiting blood
- Pregnancy with new abdominal/pelvic pain, shoulder-tip pain, fainting, or bleeding
- New bowel/bladder control problems, urinary retention, saddle numbness, or progressive leg weakness (neurologic emergency)
- Back pain after significant trauma (fall, crash) or in people with osteoporosis/cancer history
If you are unsure, treat “red flag + low back pain and stomach pain” as a reason to be evaluated promptly.
The 7 possible causes doctors warn about when low back pain and stomach pain happen together
Below are seven high-yield causes clinicians consider when a person reports low back pain and stomach pain together. The goal is not for you to self-diagnose, but to recognize patterns and know when to escalate.
1) Kidney stones (renal/ureteric colic)
Kidney stones are a classic reason people experience low back pain and stomach pain together. The stone irritates the ureter (the tube from kidney to bladder), causing intense “colicky” pain that can shift as the stone moves.
How it typically feels
- Sudden onset flank or back pain that may wrap to the lower abdomen or groin
- Pain often comes in waves; people can’t find a comfortable position
- You may also have back pain and nausea or vomiting
Other clues that support this cause
- Blood in the urine (visible or microscopic)
- Urinary urgency or burning (especially as the stone approaches the bladder)
- Pain that is not clearly linked to movement, bending, or posture changes
What doctors may do
- Urine test (blood, infection markers)
- Imaging depending on risk and setting (CT, ultrasound)
- Pain control and hydration guidance; sometimes medication to help stone passage
Seek urgent care if
- Fever/chills (stone + infection can be dangerous)
- Intractable vomiting, severe uncontrolled pain, or one kidney/known kidney disease
2) Urinary tract infection (UTI) or kidney infection (pyelonephritis)
A UTI can cause suprapubic discomfort, but when infection ascends to the kidney, it often produces flank/back pain plus abdominal discomfort—making low back pain and stomach pain a common pairing. Kidney infection is more likely to cause fever and systemic illness than a simple bladder infection.
How it typically feels
- Dull ache in the flank or low back, sometimes with lower abdominal pressure
- Burning urination, urgency, frequency
- In kidney infection: fever, chills, nausea, feeling “flu-ish”
Other clues
- Cloudy or foul-smelling urine
- Pain is often not relieved by stretching or changing positions
What doctors may do
- Urinalysis and urine culture
- Assessment for dehydration, sepsis risk, pregnancy status
- Antibiotics when indicated
Seek urgent care if
- High fever, shaking chills, confusion, severe weakness, or pregnancy with urinary symptoms
3) Acute pancreatitis (upper abdominal pain radiating to the back)
Although pancreatitis pain is usually felt in the upper abdomen, it is famously described as abdominal pain that radiates to the back. People may describe it as severe “stomach pain” plus back pain, sometimes felt lower depending on posture and body build.
How it typically feels
- Deep, severe upper abdominal pain that can bore through to the back
- Often associated with nausea/vomiting and worsens after eating
- Many people report that leaning forward or curling up provides partial relief
Other clues
- Recent heavy alcohol intake, gallbladder disease history, very high triglycerides (risk factors)
- Marked tenderness in the upper abdomen
What doctors may do
- Blood tests (lipase/amylase) and metabolic assessment
- Ultrasound/CT if needed to define cause and severity
- IV fluids, pain control, monitoring for complications
Seek urgent care if
- Pain is severe and persistent, vomiting persists, or you feel faint/confused
4) Appendicitis (including “atypical” or retrocecal appendicitis)
Appendicitis is usually right-lower abdominal pain, but the appendix can sit in positions that irritate nearby muscles (like the psoas) and nerves, producing back, flank, or even hip pain—so low back pain and stomach pain can coexist.
How it typically feels
- Pain that starts near the belly button and then localizes to the right lower abdomen (classic pattern)
- Loss of appetite, nausea, low-grade fever
- Sometimes pain with walking, hopping, or extending the right hip (psoas irritation)
Other clues
- Worsening pain over hours
- Tenderness when pressing the right lower abdomen
What doctors may do
- Focused exam, labs (white blood cell count), imaging (ultrasound/CT) as appropriate
- Surgical consult when suspected
Seek urgent care if
- Pain is steadily worsening, fever rises, or there is significant vomiting
5) Diverticulitis or other lower-bowel inflammation
Diverticulitis (inflamed pouches in the colon) is a common cause of lower abdominal pain in adults and can refer discomfort to the low back. People often describe “lower left stomach pain” plus a deep back ache—another scenario where low back pain and stomach pain occur together.
How it typically feels
- Usually left-lower abdominal pain (but location can vary)
- May be accompanied by fever, constipation, or diarrhea
- Low-grade, deep ache that can be felt in the back or pelvis
Other clues
- Pain that worsens over 1–2 days rather than minutes
- Tenderness localized to one side of the lower abdomen
What doctors may do
- Labs and imaging (often CT) depending on severity
- Antibiotics or supportive care depending on the clinical picture
- Advice on diet progression during recovery
Seek urgent care if
- High fever, severe worsening pain, vomiting, or inability to pass stool/gas
6) Gynecologic or pregnancy-related causes (endometriosis, ovarian cyst/torsion, ectopic pregnancy)
In people with ovaries/uterus, pelvic organs can generate pain that feels like low back pain and stomach pain—particularly lower abdominal cramping or pelvic pressure with a back ache. Endometriosis is a common inflammatory condition associated with pelvic pain, and flares may track with the menstrual cycle.
How it typically feels
- Cyclic pelvic pain (worse around periods) with low back pain and stomach pain
- Pain with sex, bowel movements, or urination in some cases (endometriosis patterns)
- Sudden severe one-sided pelvic pain can occur with ovarian torsion or cyst rupture
Other clues
- Late or missed period, positive pregnancy test, or unusual bleeding (consider ectopic pregnancy)
- Shoulder-tip pain, dizziness, or fainting with pregnancy-related pain is an emergency sign
What doctors may do
- Pregnancy test when relevant (this is a standard safety step)
- Pelvic exam and ultrasound
- Referral to gynecology when suspected
Seek urgent care if
- Pregnancy + new pelvic pain, fainting, heavy bleeding
- Sudden severe one-sided pelvic pain with nausea/vomiting (torsion risk)
7) Abdominal aortic aneurysm (AAA) or aortic emergency (rare but dangerous)
An abdominal aortic aneurysm is an abnormal widening of the large artery (aorta) in the abdomen. Most AAAs are silent, but if an aneurysm leaks or ruptures, it can present with severe abdominal pain and back pain. This is one of the key “do not miss” causes when clinicians hear low back pain and stomach pain together—especially in older adults and people with vascular risk factors.
For a peer-reviewed overview of abdominal aortic aneurysm definitions, risk factors, and rupture risk (and why sudden abdominal + back pain can be dangerous), see Abdominal aortic aneurysm: A comprehensive review (Aggarwal et al., 2011).
How it typically feels
- Sudden, severe abdominal pain with back pain (sometimes described as deep, tearing, or ripping)
- May be accompanied by collapse, dizziness, sweating, or shock
Other clues
- Age over 60, smoking history, known aneurysm, cardiovascular disease
- A pulsating abdominal mass may be present but is not reliable for self-checking
What doctors may do
- Emergency evaluation, rapid imaging (ultrasound/CT)
- Vascular surgery involvement immediately if suspected
Seek urgent care if
- Symptoms are sudden and severe, especially with dizziness/fainting or very low blood pressure
Quick pattern guide: matching symptom clusters to likely causes
This is not a diagnosis tool, but it helps you understand why doctors ask certain questions when you report low back pain and stomach pain.
| What stands out most | Common cluster | Why it matters |
|---|---|---|
| Waves of severe flank pain + can’t get comfortable | Stone pattern | Ureter irritation causes shifting, colicky pain |
| Fever/chills + urinary symptoms + back/flank ache | Infection pattern | Kidney infection can worsen quickly |
| Severe upper abdominal pain + vomiting + pain “through to back” | Pancreas pattern | Needs labs and fluid management |
| Migrating pain to right-lower abdomen + worsening over hours | Appendix pattern | Delay raises complication risk |
| Left-lower abdominal tenderness + fever/constipation/diarrhea | Diverticulitis pattern | Imaging guides management |
| Cyclic pelvic pain + lower back and abdominal pain | Endometriosis pattern | Inflammatory pelvic pain referral |
| Sudden severe abdominal + back pain + fainting/dizziness | Aortic emergency | Time-critical, life-threatening |
Myths vs facts about low back pain and stomach pain
- Myth: “If it hurts in the back and belly, it must be the spine.”
Fact: Many abdominal/pelvic problems refer pain to the back; you need pattern + associated symptoms. - Myth: “Gas pain can’t cause back pain.”
Fact: Bowel distension can cause back discomfort via pressure and shared nerve pathways, but it should improve and should not come with serious red flags. - Myth: “If stretching helps a little, it can’t be serious.”
Fact: Some serious conditions fluctuate. Red flags and systemic symptoms matter more than short-term relief. - Myth: “Pain location alone tells the diagnosis.”
Fact: With low back pain and stomach pain, timing, triggers, urinary/bowel symptoms, fever, and pregnancy status often matter more than the exact spot.
From the Clinic: Dr. Arora’s Expert Insight
In my clinical work, the most common mistake I see with low back pain and stomach pain is that people treat it as “either back or belly,” and they pick one strategy too aggressively. They either keep stretching and twisting because they assume it’s muscular, or they completely stop moving because they assume it’s an internal problem. Both extremes can backfire.
What works better is a two-lane approach: first, screen for danger (fever, urinary changes, worsening pain, pregnancy, fainting), and if none are present, use gentle movement as a diagnostic tool. Mechanical pain usually changes with posture, breathing, or a short walk; visceral pain often doesn’t. This simple “does it change?” test—done carefully—often clarifies the next step faster than Google searches.
What to do next: a step-by-step plan (without guessing)
If you’re experiencing low back pain and stomach pain now, use this structured approach.
Step 1: Do a 60-second safety screen
Ask yourself:
- Do I have fever, faintness, severe vomiting, blood in urine/stool, or new neurologic symptoms?
- Am I pregnant or could I be?
- Is the pain sudden and severe or rapidly worsening?
If yes to any, treat low back pain and stomach pain as urgent until proven otherwise.
Step 2: Identify your “dominant lane” (urinary, bowel, pelvic, or mechanical)
Urinary lane clues
- Burning urination, urgency, cloudy urine
- Flank pain wrapping forward
- Low back pain and stomach pain with fever/chills → higher concern
Bowel lane clues
- New constipation/diarrhea, bloating, pain around meals
- Localized lower abdominal tenderness (especially one-sided)
- Back pain and stomach cramps that track with bowel changes
Pelvic lane clues
- Cyclic symptoms around periods
- Lower back pain and pelvic pain, pain with sex, or unusual bleeding
- Pregnancy-related symptoms
Mechanical lane clues (still important)
- Pain changes clearly with bending, sitting, getting up, coughing, or lifting
- A specific movement triggers pain
- Gentle walking or position change improves symptoms
Even if mechanical features dominate, don’t ignore red flags—low back pain and stomach pain can overlap.
Step 3: Use “safe tests” that don’t aggravate symptoms
These are not medical tests—just safe observations.
- Position change test (2 minutes): Lie on your back with knees supported (pillow under knees). If low back pain and stomach pain ease notably, it suggests a mechanical component or muscle guarding.
- Short walk test (3 minutes): Walk at an easy pace. If symptoms settle, a purely internal organ cause is less likely (not impossible).
- Hydration check: If you’re dehydrated (dark urine, dry mouth), symptoms from stones, infection, or constipation can worsen.
Stop if anything makes pain worse quickly or causes dizziness.
Gentle relief measures you can start today (while arranging care)
These are conservative steps that are generally safe for many people with low back pain and stomach pain—assuming you do not have red flags.
Do
- Hydrate steadily (small sips frequently if nauseated)
- Use heat on the low back for muscle guarding (15–20 minutes)
- Choose easy meals (soups, bland foods) if nausea/bloating is present
- Keep moving lightly (short walks, gentle posture changes) rather than bed rest
Don’t
- Don’t do aggressive twisting stretches or deep forward bends when you have low back pain and stomach pain—especially if nausea, fever, or urinary symptoms are present.
- Don’t ignore worsening pain or new systemic symptoms.
- Don’t self-medicate heavily (especially NSAIDs) if you suspect dehydration, kidney issues, ulcers, or you’re unsure—speak with a clinician.
If serious causes are ruled out: a 10-minute reset for the common “guarding” pattern
After an urgent cause has been excluded, the most common reason low back pain and stomach pain keeps lingering is a protective guarding pattern: the abdominal wall, hip flexors, and low back tighten together.
10-minute reset (once or twice daily for 3–5 days)
1) 90/90 breathing (2 minutes)

- Lie on your back with calves on a chair (hips and knees about 90°).
- Inhale through the nose 4 seconds.
- Exhale slowly 6–8 seconds, letting the ribs soften down.
- Repeat 6–8 breaths.
This reduces bracing and can ease low back pain and stomach pain driven by tension.
2) Gentle pelvic tilts (2 minutes)
- Stay on your back, knees bent.
- Slowly flatten your low back into the floor (20–30% effort), then release.
- 8–10 reps.
3) Supported single-knee to chest (2 minutes)

- Bring one knee toward the chest only as far as comfortable.
- Hold 10 seconds, breathe, switch sides.
- 3–4 rounds each side.
Skip this if it increases abdominal pain.
4) Side-lying “open book” breathing (2 minutes)
- Lie on your side, knees bent, pillow between knees.
- Breathe into the side ribs; avoid deep twisting.
- 6–8 slow breaths.
5) Short walk (2 minutes)
- Easy pace, relaxed arms.
- Stop if pain spikes or you feel unwell.
Prevention stack: reduce repeats of low back pain and stomach pain
If you’ve had repeated episodes of low back pain and stomach pain, consider prevention on two tracks: spine capacity and gut/urinary triggers.
Spine capacity (weekly)
- 3–4 days/week: 15–20 minutes of gentle strength (glute bridges, bird-dog, side planks modified)
- Daily: brief mobility (hips, thoracic spine) without forcing range
- Build walking tolerance gradually
Gut/urinary triggers
- Hydration habits (especially during travel, workouts, hot weather)
- Fiber consistency (increase slowly; avoid sudden large jumps)
- Don’t delay urination for long periods
- Review recurrent UTI or stone risk factors with your clinician
Frequently asked questions about low back pain and stomach pain
1) Can low back pain and stomach pain be “just gas”?
It can be, especially if you have bloating, relief after passing gas or a bowel movement, and no red flags. However, persistent or severe low back pain and stomach pain—especially with fever, vomiting, or urinary changes—should be evaluated.
2) How do I tell kidney stone pain from a back muscle strain?
Stone pain often comes in waves, makes you restless, and may radiate toward the groin; muscle strain is more position- and movement-dependent. Blood in urine, nausea, and low back pain and stomach pain that doesn’t change with posture increase suspicion of a stone.
3) Can a UTI cause low back pain and stomach pain without burning urination?
Yes. Some people—especially older adults—may not notice classic burning. If you have low back pain and stomach pain with fever, chills, flank tenderness, or feeling very unwell, get assessed for kidney infection.
4) Why does pancreatitis feel like back pain?
The pancreas sits deep in the upper abdomen near the spine. Inflammation can produce abdominal pain that radiates to the back, so people describe low back pain and stomach pain even when the main source is upper abdominal.
5) Can endometriosis cause back and stomach cramps?
Yes. Endometriosis-related inflammation and pelvic floor guarding can produce lower back and abdominal pain, often worse around periods. If low back pain and stomach pain is cyclic and accompanied by heavy periods, pain with sex, or infertility concerns, discuss evaluation options.
6) Is low back pain and stomach pain in early pregnancy normal?
Mild aches can occur, but you should never assume. If you are pregnant (or could be) and have low back pain and stomach pain with bleeding, fainting, shoulder-tip pain, or one-sided pelvic pain, seek urgent care to rule out ectopic pregnancy.
7) When should I get imaging?
Imaging depends on the pattern and risk. Low back pain and stomach pain with fever, blood in urine, suspected appendicitis/diverticulitis, pancreatitis complications, or an aortic emergency often requires prompt imaging. Mechanical back pain without red flags usually does not need immediate imaging.
8) What if the pain is on the right side only?
Right-sided low back pain and stomach pain raises suspicion for appendicitis, right kidney stones, or gallbladder/liver issues depending on the exact location and symptoms. If it is worsening, associated with fever, vomiting, or localized tenderness, seek evaluation.
9) Can constipation cause low back pain and stomach pain?
Yes. Constipation can cause back pressure and abdominal cramping, and it can also trigger muscle guarding in the low back. If symptoms resolve with bowel movement and there are no red flags, conservative care is reasonable. If constipation is new, severe, or accompanied by weight loss, blood in stool, or severe pain, get assessed.
10) What’s the safest first step if I’m unsure?
Start with the red-flag screen, then focus on hydration, gentle movement, and arranging medical advice. If low back pain and stomach pain is severe, sudden, or accompanied by systemic symptoms, treat it as urgent.




