If you are dealing with a stubborn gut and a sore back at the same time, it is reasonable to wonder: can constipation cause lower back pain. For many people, the timing is too consistent to feel like coincidence—no bowel movement for a day or two, then a heavy, tight ache across the beltline.
The short answer is yes, constipation can contribute to lower back pain in several very real, body-mechanics ways. If you have been searching can constipation cause lower back pain repeatedly, it is usually because your body is giving you a consistent pattern worth decoding.
But constipation is not the only explanation, and sometimes back pain that “feels like constipation” is a sign you should not ignore.
This guide explains the gut–spine link in plain language, helps you self-check what is most likely driving your symptoms, and gives a stepwise reset plan you can try at home.

Can constipation cause lower back pain? Yes—here’s the physiology
When you ask can constipation cause lower back pain, think of it as a pressure-and-coordination problem, not just a “bathroom problem.”
When people ask can constipation cause lower back pain, they are usually describing one of three patterns: pressure pain, muscle guarding, or referred pain. Often, more than one mechanism is happening at once.
1) Pressure and distension: the “fullness” that tugs on your back
Yes, can constipation cause lower back pain simply from buildup and stretch in the colon? For many bodies, that is the main mechanism.
Constipation can lead to stool building up in the colon (large intestine). As the colon fills, it can distend—meaning it stretches and becomes more pressurized. That distension can create a deep, dull ache that feels like it sits in the low back, especially around the sacrum (the bony area above the tailbone). If you have a bloated abdomen at the same time, pressure-related back pain becomes even more plausible.
Why this can feel like back pain:
- The colon and rectum sit close to the pelvis and the lower spine.
- Distension increases pressure in the abdomen and pelvis.
- That pressure can change how you hold your posture and how your back muscles “brace.”
2) Muscle guarding: when your core tightens to protect a sensitive belly
When your belly feels tight or painful, your body often responds by stiffening the abdominal wall and pelvic muscles. This is called guarding—an automatic protective strategy. Guarding can reduce spinal motion, increase lumbar stiffness, and overload the muscles that run along the spine.
So yes: can constipation cause lower back pain through muscle guarding? Absolutely. In fact, many people notice their back feels “locked” until they finally pass stool and the abdominal tension eases.
3) Referred pain: one area feels it, another area causes it
Referred pain is when the brain interprets signals from one area as pain in a nearby or related region. The nerves that carry sensation from pelvic organs and the lower back share pathways. That overlap can blur the location of discomfort.
This is why can constipation cause lower back pain is not a weird question—it is a nervous-system question as much as a bowel question.
4) Pelvic floor involvement: the constipation–back pain loop
Your pelvic floor is a sling of muscles at the bottom of the pelvis. It helps with bowel control and coordinates with the diaphragm and deep core for stability. If the pelvic floor is too tight, poorly coordinated, or fatigued, you can get:
- Straining and incomplete emptying
- Tailbone or sacral ache
- Low back tightness, especially after attempts to go
In this loop, constipation can trigger back pain, and back pain can make constipation worse by reducing comfortable movement and increasing muscle tone.
What a tight or poorly coordinated pelvic floor can feel like
People rarely describe it as “pelvic floor tightness.” Instead, they notice practical signs: you have to strain even when stool feels close, you cannot relax “down there,” you feel pressure near the tailbone, or you finish but still feel like something is left.
Why coordination matters for the low back
During a bowel movement, the pelvic floor should soften and lengthen (relax) while the abdominal wall creates gentle pressure. If the pelvic floor stays braced, your body often compensates by tightening the low back and holding the breath. Over time, that compensation can make lower back pain from constipation feel like a recurring “back problem,” even when the root issue is emptying mechanics.
What constipation-related lower back pain usually feels like

If you are still asking can constipation cause lower back pain in your specific case, check whether your symptoms match these common features:
- Timing: Back pain increases when you have not had a bowel movement, and eases after you finally go.
- Quality: Dull, heavy ache or pressure; sometimes a band-like tightness across the lower back.
- Location: Centered low back, sacrum, tailbone, or a broad area rather than a sharp pinpoint.
- Associated gut signs: Bloating, gas, abdominal discomfort, reduced appetite, or feeling “full.”
- Movement effect: Gentle walking or a warm shower helps; sitting still often worsens stiffness.
Not every case follows this exact pattern, but the more boxes you tick, the more reasonable the “yes” becomes.
When the answer is “maybe”: other common reasons your gut and back flare together
People often ask can constipation cause lower back pain when the true driver is shared triggers that affect both systems.
Dehydration and low fiber
Not enough fluid can harden stool. Low fiber can reduce stool bulk and slow movement through the gut. Both can coincide with lower activity, long sitting hours, and back stiffness.
Stress and the gut–muscle connection
Stress changes bowel motility and increases muscle tone. A tense nervous system can tighten the pelvic floor and the low back at the same time.
Medications and supplements
Many common medicines can slow the gut, and some can also affect muscles or hydration status. Examples include certain pain medicines, iron supplements, and some allergy or mood medicines. If constipation began after a new medication, it is worth discussing with the prescriber.
Less movement
Reduced daily walking and prolonged sitting can slow bowel motility and also load the lumbar spine. In these scenarios, can constipation cause lower back pain is partly true—but the bigger picture is a sedentary routine.
Quick self-check: is constipation likely the main driver of your back pain?
If your main question is still can constipation cause lower back pain, this section helps you separate a likely gut-driven flare from a back issue that just happens to coexist.
Use this “probability checklist.” It does not diagnose anything, but it can guide your next steps.
Higher likelihood it is constipation-related
- Back pain clearly spikes on days you are constipated
- You feel abdominal pressure or bloating with the back ache
- Pain improves within hours after a good bowel movement
- You have to strain, stools are hard, or you feel incomplete emptying
- Your back pain is more “pressure/tightness” than “electric/shooting”
Lower likelihood it is constipation-related
- Pain is sharp, shooting down the leg, or associated with numbness/tingling
- You have fever, vomiting, or severe abdominal pain
- You see blood in stool or have black/tarry stools
- Back pain wakes you from sleep consistently and is not linked to bowel timing
- You have unintentional weight loss or a new change in bowel habits lasting weeks
If you are unsure, keep a simple two-week log: bowel movement frequency, stool hardness, bloating, and back pain score. Patterns often become obvious.
Why constipation can flare one-sided back pain
A frequent follow-up to can constipation cause lower back pain is: “Why is it worse on one side?” The colon is not perfectly centered. Gas pockets and stool load can create asymmetrical pressure. Plus, many people have side-dominant postures—crossing legs, leaning, or twisting while sitting—which can make a pressure problem feel one-sided.
The 48-hour reset plan: what to do first (without overcomplicating it)
This plan is designed for the common scenario where can constipation cause lower back pain because pressure and muscle guarding build up together over 24–72 hours.
If you believe can constipation cause lower back pain for you, the best first step is often to reduce pressure, improve motility, and calm muscle guarding—gently.
Step 1: Hydrate in a structured way
Instead of chugging water once, spread fluids across the day. Pair water with regular meals and snacks. If you are sweating heavily or ill, consider oral rehydration solutions as advised by a clinician.
Step 2: Add “easy fiber” before “heavy fiber”
Some people worsen bloating by jumping straight to large amounts of bran or raw salads. Start with softer, easier options:
- Oats
- Cooked vegetables
- Chia in small amounts
- Prunes or kiwi for some people
If gas is a major issue, scale slowly.
Step 3: Walk in short bouts
A 10–15 minute walk after meals can stimulate gut movement and reduce lumbar stiffness. If you are very sore, do 3–5 minutes, several times.
Step 4: Use a toileting posture that helps emptying
Elevate your feet on a small stool so your knees are above your hips. Lean forward with elbows on thighs. Relax your belly. Avoid breath-holding strain.
A 60-second toilet technique

- Set feet on a stool and let your knees rise.
- Inhale gently through the nose so the belly softens outward.
- Exhale slowly and imagine the pelvic floor “dropping” rather than pushing.
- If nothing happens in a few minutes, stand up, walk, and try again later.
👨⚕️ Dr. Arora’s Clinical Note:
Many patients ask me if they should “push harder” when they feel backed up—especially when the low back is already aching. Counter-intuitively, the quickest way to reduce constipation-related low-back tightness is often to reduce bracing first, not increase effort.
Physio secret (60–90 seconds before you try again):
- Set up: Sit with feet on a stool (knees above hips), lean forward, elbows on thighs.
- Inhale: Inhale quietly through the nose so the belly softens outward (no chest lifting).
- Exhale: Exhale slowly for 6–8 seconds (as if fogging a mirror) and think: “tailbone heavy, sit bones widen.”
- Check: If your low back clenches during the exhale, you’re still bracing—dial down effort until the back stays quiet.
This “long exhale + pelvic drop” pattern often improves emptying mechanics and takes the “locked” feeling out of the lumbar muscles within minutes. If you regularly have to strain or feel incomplete emptying, that strongly suggests a coordination issue (dyssynergic defecation)—a pelvic floor physio assessment can be genuinely high-yield.
Step 5: Heat + gentle mobility to reduce guarding
Try a warm pack over the lower abdomen or low back for 10–15 minutes, then do gentle movements:
- Cat–camel (slow)
- Pelvic tilts
- Child’s pose if comfortable
- Easy hip flexor stretch (no forcing)
The goal is not a “back workout.” The goal is to signal safety to the nervous system so muscles stop bracing.
Two movement rules that prevent flare-ups
- Keep everything in a comfortable range. Mild stretch is fine; sharp pain is not.
- Move slowly enough that you can breathe normally the whole time.
Step 6: Decide if an over-the-counter option is appropriate
If constipation is persistent, some people use OTC remedies. Because the right choice depends on your age, medical history, pregnancy status, and symptoms, it is best to follow product guidance and speak with a pharmacist or clinician—especially if you have new constipation or are using laxatives frequently.
“Constipation and back pain” patterns by age and life stage
Can constipation cause lower back pain across life stages? Yes, but the most likely drivers shift with routine, hormones, mobility, and medications.
Can constipation cause lower back pain in children, adults, and older adults? Yes, but the context differs.
Children and teens
In kids, constipation can show up as belly pain, irritability, reduced appetite, and sometimes back or hip discomfort. Stool withholding (avoiding the toilet) is common. If a child has severe pain, vomiting, fever, or is not passing gas, seek urgent care.
Working-age adults
The most common drivers are routine-based: long sitting, low fiber, low hydration, stress, travel, and irregular toilet timing. Lower back pain from constipation in this group is often posture-and-pressure related.
Pregnancy and postpartum
Hormone shifts can slow bowel motility, and pelvic floor changes can alter emptying mechanics. Back pain is also common for musculoskeletal reasons. If you are pregnant and asking can constipation cause lower back pain, the answer is often “yes, but we must also screen for pregnancy-specific red flags.” Discuss new or severe symptoms with your obstetric team.
Older adults
Constipation can be influenced by medications, reduced mobility, dehydration, and medical conditions. New constipation with back pain in older adults should be taken seriously, especially if accompanied by weight loss, anemia, or appetite changes.
The gut–spine link explained in one picture (conceptually)
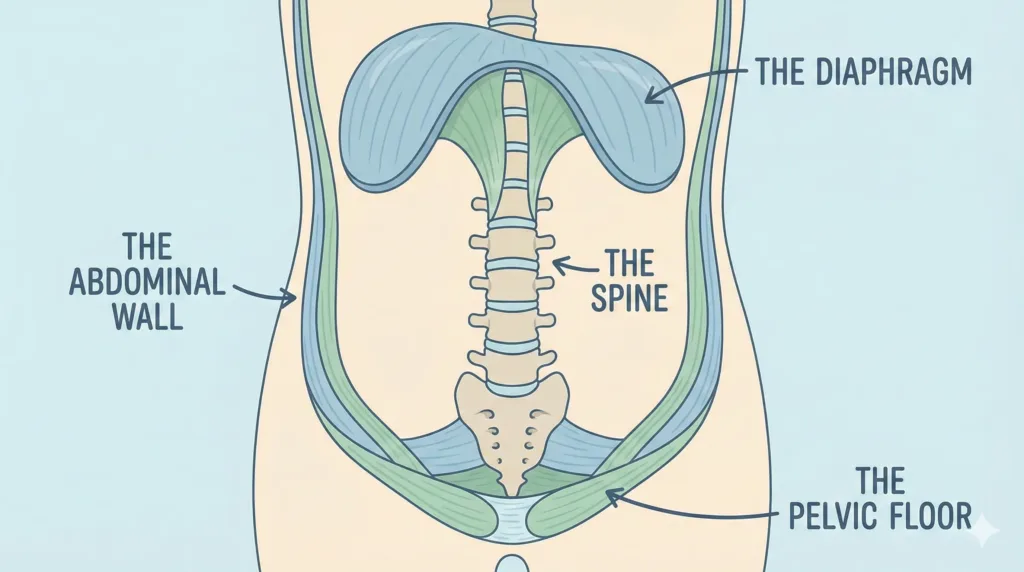
Think of your trunk like a pressure cylinder:
- The diaphragm on top
- The pelvic floor on the bottom
- The abdominal wall around the sides
- The spine as the central support
When the gut is distended, pressure rises in the cylinder. If the pelvic floor and abdominal wall brace, the spine can feel compressed. This is one of the simplest ways to understand why can constipation cause lower back pain without invoking anything mysterious.
Red flags: when back pain with constipation needs urgent evaluation
It is important to say this clearly: sometimes the “can constipation cause lower back pain” question delays care for a different problem.
Seek urgent medical evaluation if you have:
- Severe, worsening abdominal pain, repeated vomiting, or inability to pass gas
- Fever, chills, or feeling very unwell
- New weakness, numbness in the groin/saddle area, or loss of bowel/bladder control
- Blood in stool, black stools, or significant rectal bleeding
- Back pain after a fall or injury, especially in older adults
- Unexplained weight loss, persistent night pain, or a change in bowel habits lasting weeks
These do not automatically mean something serious, but they do mean “do not self-manage only.”
A practical “do / don’t” table for fast relief
| Do | Don’t |
|---|---|
| Walk in short bouts after meals | Stay immobile all day “to rest the back” |
| Use a footstool for better toileting posture | Force breath-holding strain on the toilet |
| Increase fiber gradually | Jump to extreme fiber overnight |
| Use heat to calm guarding | Aggressively stretch into sharp pain |
| Track patterns for 1–2 weeks | Guess and change everything at once |
Midpoint check: how to know your plan is working
If can constipation cause lower back pain is true for you, you should see changes in two directions:
- Bowel metrics: easier stool passage, less straining, less bloating
- Back metrics: reduced pressure ache, improved ease of movement, less morning stiffness
Improvement is often incremental. Many people feel “lighter” first, then notice their back relaxes.
For a reliablFor clinician-grade, primary evidence on constipation management (including stepwise OTC and prescription options), see the gastroenterology guideline [American Gastroenterological Association–American College of Gastroenterology Clinical Practice Guideline: Pharmacological Management of Chronic Idiopathic Constipation, 2023].e medical overview of constipation symptoms and causes.
If the back pain feels like sciatica: what constipation can and cannot do
If you are asking can constipation cause lower back pain and leg symptoms, you are not alone. The key is to distinguish pressure-and-guarding effects from true nerve compression.
A common worry is: can constipation cause lower back pain that shoots down the leg. Constipation can increase pelvic pressure and muscle guarding, which may irritate sensitive tissues and make existing nerve symptoms feel worse. But classic sciatica—sharp, electric pain down the leg, tingling, or numbness—often points to a spine or nerve issue that should be assessed separately.
A simple distinction:
- Pressure/ache that changes with bowel movement: constipation link more likely
- Radiating leg symptoms with cough/sneeze sensitivity: nerve involvement more likely
Both can coexist, especially if you are already prone to disc irritation or tight hip muscles.
Myths vs facts
| Myth | Fact |
|---|---|
| “Back pain means it can’t be constipation.” | Constipation can create pressure, guarding, and referred pain that feels like low back pain. |
| “If I’m constipated, my back pain is always from my gut.” | You can have constipation and a separate back problem at the same time. |
| “More fiber is always the answer.” | Too much fiber too fast can worsen bloating; gradual changes work better. |
| “Straining is normal if you’re busy.” | Frequent straining can worsen pelvic floor coordination and prolong constipation. |
A stepwise plan for recurring episodes
If can constipation cause lower back pain is a recurring theme in your life, treat it like a recurring systems issue: bowel mechanics plus movement habits plus stress physiology.
If you keep returning to the same question—can constipation cause lower back pain every few weeks—build a prevention stack that fits your real life.
Step A: Make bowel habits predictable
- Pick a consistent “toilet window,” often after breakfast.
- Give yourself unhurried time.
- Avoid scrolling and rushing; these increase straining.
Step B: Build movement into the day
- Short walks are often more sustainable than long workouts.
- Break sitting every 30–45 minutes with 1–2 minutes of standing or pacing.
Step C: Support the pelvic floor and core coordination
You do not need intense core training. Instead, focus on coordination:
- Slow nasal breathing into the lower ribs
- Gentle belly expansion on inhale
- Relaxation of the pelvic floor (think “softening”) on exhale
If constipation is long-standing and you feel incomplete emptying often, pelvic floor physical therapy assessment can be transformative.
Step D: Food triggers, simplified
Rather than obsessing over every food, look for patterns:
- Low fruit/vegetable days
- Travel days
- Low fluid days
- High ultra-processed days
- Irregular meal timing
Small consistency beats a perfect diet for three days.
Frequently Asked Questions
1. Can constipation cause lower back pain even if my stools aren’t very hard?
Yes. You can be constipated through infrequent bowel movements, incomplete emptying, or significant bloating and gas—even if stool is not rock hard. Pressure and muscle guarding can still drive discomfort.
2. Can constipation cause lower back pain on the left side specifically?
It can. The descending and sigmoid colon sit more on the left, so stool load and gas can create left-sided pressure. Posture and muscle dominance can amplify that side.
3. Can constipation cause lower back pain after eating?
Often, yes. Eating triggers a normal reflex that stimulates the colon. If stool is backed up, that reflex can increase cramping, bloating, and pressure sensations that refer to the lower back.
4. Can constipation cause lower back pain during your period?
It can. Hormone shifts can change bowel motility and pain sensitivity. Pelvic pressure may rise, and muscle guarding can increase. If pain is severe, new, or associated with heavy bleeding, seek evaluation.
5. Can constipation cause lower back pain that feels sharp?
Constipation-related pain is more often dull and pressure-like, but sharp pain can occur with intense cramping, gas pockets, or significant pelvic floor spasm. Sharp, persistent pain should be assessed for other causes too.
6. Can constipation cause lower back pain and nausea at the same time?
It can, especially when bloating and gut slowdown are significant. However, nausea with severe abdominal pain, vomiting, fever, or inability to pass gas is a red flag and should be evaluated urgently.
7. Can constipation cause lower back pain and urinary pressure?
Yes. A full rectum can increase pelvic pressure and make you feel urinary urgency or pressure. If you have burning urination, fever, or flank pain, consider a urinary issue and seek care.
8. How long does constipation-related back pain take to go away?
Some people feel relief within hours after a good bowel movement. Others need a few days of hydration, movement, and gradual fiber increases to reduce distension and muscle guarding.
9. What is the fastest safe way to test whether constipation is the cause?
Track timing: if your back pain reliably worsens with constipation and eases after bowel movement, the link is likely. Combine that with bloating and straining history. If you have red flags, do not “test”—get assessed.
10. When should I see a clinician about constipation and lower back pain?
If symptoms are new and persistent, if you need laxatives frequently, if there is blood in stool, significant weight loss, ongoing night pain, fever, vomiting, or neurologic symptoms, seek medical evaluation.
The most useful takeaway
If you came here with one question—can constipation cause lower back pain—you now have a clearer map of how and why it can happen, and how to respond safely.
So, can constipation cause lower back pain? Yes—through pressure, guarding, referred pain, and pelvic floor mechanics. The most practical approach is to treat it like a two-system issue: reduce gut pressure while calming the muscles that brace around it.
When the pattern is clear, simple steps—hydration, gradual fiber, walking, toileting posture, and gentle heat/mobility—often produce meaningful relief. And when the pattern is not clear, red-flag screening and timely evaluation protect you from missing something important.




