“Expert Review: This article includes clinical insights from Dr. Arora, a physiotherapist with 20+ years of experience.”
If you keep searching tight glutes and lower back pain, you are not alone. It’s one of the most common “two-for-one” complaints: your butt feels like a rock, and your lower back feels compressed, pinchy, or tired—especially after sitting, walking, or lifting.
Here’s the key: tight glutes and lower back pain is often not a simple “my glutes are short, so I must stretch” problem. In many people, the glutes feel tight because they are protecting something (a sensitive joint, an irritated disc, a reactive nerve, or a hip that isn’t sharing load well). In other cases, they feel tight because they are overworking—trying to stabilize the pelvis when other systems (hips, trunk control, breathing mechanics, or foot/ankle control) are not doing their job.
This guide breaks down the real mechanics behind tight glutes and lower back pain, the patterns I see most often, and the fix most people miss: restoring hip-driven movement and glute capacity without provoking your back.
Important: This is educational information, not a diagnosis. If you have red flags (listed below), seek urgent medical care.

Before we start: quick safety check (red flags)
Most cases of tight glutes and lower back pain are mechanical and improve with conservative care. Seek urgent medical evaluation if you have any of the following:
- New trouble controlling bladder or bowel function, or numbness in the “saddle” area.
- Progressive leg weakness, foot drop, or rapidly worsening numbness.
- Fever, chills, unexplained weight loss, history of cancer, or immune suppression with new back pain.
- Recent major trauma (fall, crash) or severe unrelenting pain at rest.
- Night pain that is escalating and not position-dependent.
If you are unsure, get assessed—especially if the symptoms are new, severe, or changing quickly.
The map: why glutes and the low back “argue”
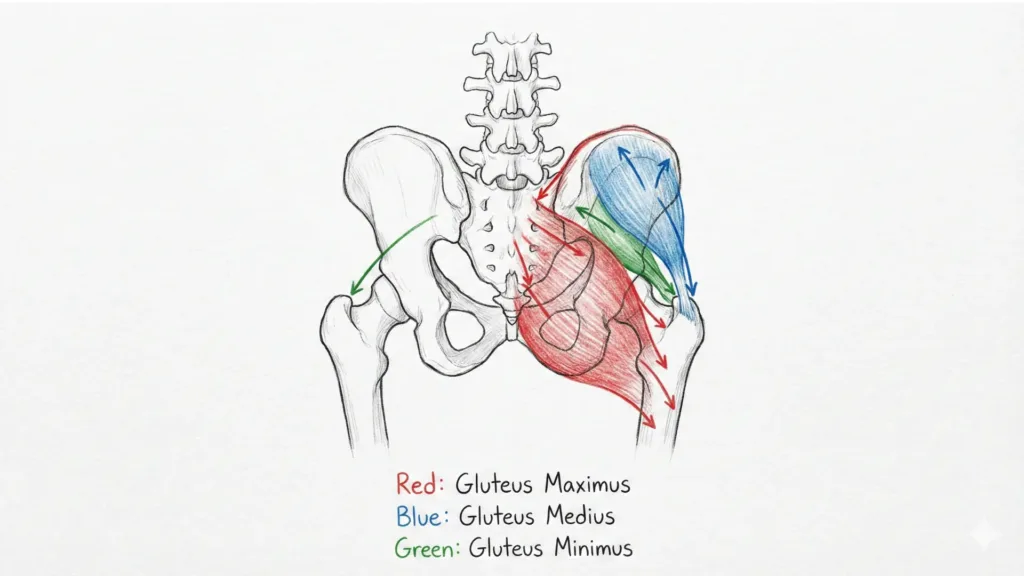
Your pelvis is the bridge between your spine and your legs. The glutes (gluteus maximus, medius, and minimus) help control this bridge in three big ways:
- Extension power: pushing you up from a chair, climbing stairs, deadlifting, sprinting (mostly glute max).
- Pelvic stability: keeping the pelvis level when you stand on one leg, walk, or run (mostly glute med/min).
- Rotation control: stopping the pelvis from twisting excessively when you turn or step (glutes + deep rotators).
When the hip cannot produce or control force efficiently, the lumbar spine often “pays the bill.” That’s why tight glutes and lower back pain frequently show up together.
A plain-English note on “tightness”
“Tight” can mean different things:
- Short/tissue tightness: the muscle is actually shortened (less common than people think).
- Protective tone (guarding): the nervous system increases tension to protect a sensitive area.
- Trigger points: small hypersensitive spots that can refer pain into the butt, hip, or low back.
- Overuse fatigue: the muscle is working too hard, too often, because something else is not contributing.
So when you feel tight glutes and lower back pain, the right question is not “what stretch?” It’s “why is my system choosing tension?”
Part 1 — The Problem: 9 real causes of tight glutes and lower back pain
1) Hip extension loss (your hip can’t go back, so your back goes back)
One of the most common drivers of tight glutes and lower back pain is limited hip extension—your thigh cannot move behind you smoothly. When you walk, climb, or stand up, the body still needs extension somewhere. If the hip is “blocked,” the lumbar spine extends instead.
Common clues
- Low back feels compressed during walking uphill or after standing.
- Glutes feel tight after sitting, then worsen when you stand.
- You arch your back to “get the leg behind you.”
Quick self-check
- Do a gentle split-stance lunge and squeeze the back-side glute. If your low back arches to find the stretch, the hip is not extending cleanly.
What helps
- Hip flexor mobility with a glute squeeze (not aggressive lumbar arching).
- Re-learning a hip hinge so extension comes from the hip, not the spine.
This is a classic “after sitting” pattern of tight glutes and lower back pain: sitting biases hips into flexion and the system loses extension capacity. It’s also why people describe it as tight glutes causing lower back pain—because the real issue is often the hip not sharing extension load.
2) Weak or delayed glute medius (pelvic drop = back tension)
When the gluteus medius is weak, delayed, or easily fatigued, the pelvis can drop or rotate during single-leg tasks like walking, stairs, and standing on one leg. Your lumbar muscles often tighten to “hold the pelvis,” and you feel tight glutes and lower back pain—commonly worse on one side.
Large clinical and research samples show hip abductor weakness is common in people with chronic non-specific low back pain [Prevalence of gluteus medius weakness in people with chronic nonspecific low back pain, 2016], and a systematic review describes measurable differences in gluteus medius function between people with and without low back pain [Gluteus medius muscle function in people with and without low back pain, 2019].
Common clues
- Pain or tightness is worse on one side.
- Standing on one leg feels shaky.
- You get outside-hip ache plus low back tightness.
Quick self-check
- Single-leg stance for 20–30 seconds. If your pelvis drops or you lean your trunk to stay balanced, glute med control may be the limiter.
What helps
- Side-lying hip abduction progressions, step-down control, and lateral walking—done with form, not speed.
3) The “stretch-only trap” (tightness from guarding, not shortness)
Many people stretch their glutes daily and still have tight glutes and lower back pain. That usually means the glutes are guarding. In response to irritation within a joint, disc, or nerve, the nervous system often induces rigidity in the pelvic and hip regions as a defensive measure.. Stretching can feel temporarily relieving but quickly rebounds—or even irritates symptoms.
Common clues
- Stretching feels good in the moment but symptoms return within hours.
- Your back feels “unstable” or “fragile.”
- You feel better with gentle movement than deep stretching.
What helps
- Lower the threat first: breathing, gentle isometrics, and graded loading.
- Treat tight glutes and lower back pain as a capacity problem, not a flexibility problem.
4) SI joint irritation (the pelvis joint that makes glutes clamp down)
The sacroiliac (SI) joints connect the sacrum to the pelvis. They are designed for small movements and load transfer. When the SI area is irritated (often after a sudden twist, pregnancy/postpartum changes, or a load spike), the glutes can “splint” the area. That produces tight glutes and lower back pain that is often one-sided and close to the dimples above the butt.
Common clues
- Pain is near one SI joint, sometimes radiating into the butt.
- Rolling in bed, standing from sitting, or single-leg loading aggravates it.
- You feel “stuck” rather than “pulled.”
What helps
- Temporary reduction of aggravating asymmetrical loads.
- Glute med endurance and trunk control to improve load transfer.
- If severe or persistent, a clinician can help differentiate SI pain from lumbar and hip sources.
[INSERT REAL PHOTO OF SPINE MODEL HERE: show the sacrum and the SI joints; point to the “dimple area” where SI pain is often felt.]
5) Disc sensitivity + bending intolerance (glutes tighten to stop motion)
Some low back pain is driven by disc sensitivity. When discs or related structures are irritated, your body can reduce motion by increasing muscle tension around the pelvis and hips. You experience tight glutes and lower back pain, but the glute tightness is secondary.
Common clues
- Pain increases with bending/lifting or prolonged sitting.
- Symptoms can radiate into the butt or thigh.
- You feel stiff after sitting, then “unlock” after walking.
What helps
- Reduce repeated bending under load temporarily.
- Use hip hinge strategies, shorter lever lifting, and gradual exposure.
- If leg symptoms are increasing, get assessed.
6) Deep gluteal pain (piriformis and friends) that mimics sciatica
Deep butt pain can irritate nearby tissues and sometimes mimic sciatica-like symptoms. People commonly label this as piriformis tightness and lower back pain, but the label is less important than identifying whether symptoms are muscular referral, nerve irritation, or lumbar referral. A critical point: butt pain radiating down the leg is not automatically a “piriformis problem.” Differential diagnosis matters, and piriformis syndrome remains a debated/variable diagnosis [Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment, 2019].
Common clues
- Deep butt pain, worse with prolonged sitting.
- Pain can refer down the back of the thigh.
- Tenderness deep in the butt; stretching sometimes worsens symptoms.
What helps
- Avoid aggressive deep stretching if it reproduces tingling, numbness, or burning.
- Improve hip rotation control and glute med endurance.
- If symptoms travel below the knee or weakness appears, seek evaluation.
7) Hip joint mechanics (limited rotation, stiff capsule, or impingement pattern)
If the hip joint is limited (for example, reduced internal rotation, a stiff capsule, or an impingement pattern), you may compensate through the lumbar spine and pelvis. Over time, that can create tight glutes and lower back pain, especially during squats, deep sitting, or twisting.
Common clues
- Pinch in the front of the hip with deep flexion.
- You can’t rotate the hip well.
- Back tightness increases after squats or long sitting.
What helps
- Hip-friendly squat depth, stance adjustments, and hip mobility drills that do not jam the hip.
- Strengthening in the range you own, then expanding range gradually.
8) Poor hip hinge and bracing strategy (your back muscles do the job of your hips)
A very common movement error: bending by rounding or arching the low back instead of hinging at the hips. Another: “over-bracing” the trunk so hard that the glutes never load properly. Both can drive tight glutes and lower back pain because you never distribute load through the hips.
Common clues
- Back tightness after lifting, gardening, or picking up kids.
- Glutes feel “offline” during bridges or squats.
- Hamstrings feel tight after light tasks.
What helps
- Rebuild hinge mechanics with simple feedback drills.
- Learn to brace “just enough,” then push through the hips.
9) Load spikes + deconditioning (capacity mismatch)
Sometimes the cause of tight glutes and lower back pain is simply a mismatch between what you did and what your tissues were prepared for: a sudden increase in steps, a new workout, a long drive, or a weekend of lifting and twisting. The glutes clamp as they fatigue; the back tightens to stabilize.
Common clues
- Symptoms flare after a new activity or longer-than-usual day.
- Pain improves with consistent, graded activity.
- Tightness becomes predictable when you track load.
What helps
- Gradual progression: increase volume 10–20% weekly rather than doubling.
- Prioritize sleep, walking, and basic strength before advanced drills.
Symptoms and patterns you may recognize
Tight glutes and lower back pain commonly shows up as one of these patterns:
- After sitting: butt feels tight when you stand; back feels stiff for the first few minutes.
- During walking: back tightness builds as stride length increases (often hip extension loss).
- One-sided: one butt feels tighter with one-sided low back ache (often pelvic control issue).
- With “sciatica-like” symptoms: butt pain with leg referral (needs differential assessment).
- After lifting: back tightness dominates; glutes feel “not firing” (hinge and loading issue).
Myths vs facts
- Myth: Tight glutes and lower back pain means you must stretch more.
Fact: Often you need better hip extension, hip control, and glute capacity—not deeper passive stretching. In other words, glute tightness and low back pain are frequently about control and tolerance, not “short” muscles. - Myth: Butt tightness is always piriformis syndrome.
Fact: Many structures can refer pain into the butt; true nerve irritation needs careful evaluation [Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment, 2019]. - Myth: If imaging is “normal,” the pain must be “just muscles.”
Fact: Pain can be significant even with minimal imaging findings, and many imaging findings are age-related. Your plan should be guided by symptoms and function, not fear.
From the Clinic: Dr. Arora’s Expert Insight
In my clinic I have seen many times that, the people who struggle most with tight glutes and lower back pain are often the most disciplined stretchers. They can do a perfect figure-4 stretch and hold it for two minutes—yet they still feel “tight” by lunchtime. Upon examination I typically find is not a shortage of flexibility, but a shortage of hip contribution: the hip doesn’t extend well when they walk, and the pelvis isn’t stable on one leg. So their nervous system chooses tension as a backup plan.
The standard advice “stretch your glutes and strengthen your core” often fails because it misses the order of operations. If you strengthen without restoring hip options, the low back keeps substituting. If you stretch a guarding system aggressively, you can irritate it further. The turning point is usually when we (1) calm the protective tone, (2) restore hip extension without lumbar compensation, and (3) build glute endurance so the pelvis stops needing a constant “clamp.” When those three pieces are in place, tight glutes and lower back pain starts fading instead of bouncing back.
Part 2 — The Solution: the fix most people miss
The fix most people miss for tight glutes and lower back pain is this: stop treating tightness as the main problem and start treating hip capacity and pelvic control as the main goal. Stretching can still help, but stretching is the garnish—not the meal.
Below is a structured plan you can follow. If anything increases sharp pain, tingling, or worsening leg symptoms, stop and get assessed.
Step 1: Calm the system (2–5 minutes, 1–3 times/day)
When tight glutes and lower back pain is driven by guarding, the first step is reducing threat and compression.
1A) 90/90 breathing reset (back-friendly)

How to do it
- Lie on your back with calves on a chair (hips and knees about 90 degrees).
- Place one hand on your lower ribs, one on your lower abdomen.
- Inhale through the nose for ~4 seconds, letting ribs expand gently sideways.
- Exhale slowly for ~6–8 seconds as if fogging a mirror, letting the ribs drop.
- Do 5–8 slow breaths.
Why it helps
This can reduce excessive extension tone and give the hips a chance to “let go.”
1B) Glute isometric “set” (no movement, just activation)
How to do it
- Stay on your back, knees bent, feet on the floor.
- Gently squeeze both glutes at 30–40% effort (not a max squeeze).
- Hold 10 seconds while breathing normally, then relax.
- Repeat 6–8 times.
Isometrics are often tolerated even when stretching flares tight glutes and lower back pain.
Step 2: Restore hip motion without feeding the back (daily)
2A) Hip flexor stretch with posterior tilt (the safe version)

How to do it
- Before moving forward, gently tuck the pelvis (think “belt buckle up”).
- Half-kneel (one knee down, one foot forward).
- Squeeze the down-knee side glute.
- Shift forward slightly until you feel a stretch in the front of the hip—not in the low back.
- Hold 20–30 seconds, repeat 2–3 times per side.
This matters most for tight glutes and lower back pain after sitting, because hip flexors are often “on” all day. If you’ve noticed tight hip flexors and tight glutes lower back pain together, think “hip extension is missing,” not “I just need to stretch harder.”
2B) Adductor rock-back (hips, not spine)

How to do it
- On hands and knees, extend one leg out to the side (knee straight or slightly bent).
- Keep spine neutral and ribs down.
- Rock hips back toward heels until you feel a stretch in inner thigh/groin.
- Rock forward again. Do 8–10 reps per side.
This improves hip options so the back doesn’t substitute, which reduces tight glutes and lower back pain during daily movement.
Step 3: Build glute capacity (3 days/week, 15–25 minutes)
Clinical exercise studies show that combining hip/glute strengthening with stabilization can improve pain and function in chronic low back pain populations [The effects of gluteus muscle strengthening exercise and lumbar segmental stabilization exercise on low back pain, 2015].
The goal is to make the glutes strong and enduring enough that they stop “panic-gripping,” which reduces tight glutes and lower back pain over time.
3A) Bridge progression (glute max)

Level 1: Basic bridge
- Lie on your back, knees bent, feet hip-width.
- Lightly brace abdomen (as if tightening a belt one notch).
- Push through heels and lift hips until shoulders–hips–knees form a line.
- Hold 2 seconds, lower slowly (3 seconds down).
- Do 2–3 sets of 8–12 reps.
Form cues
- You should feel glutes more than low back.
- If hamstrings cramp, bring heels slightly closer and reduce height.
- If your back pinches, reduce range and focus on ribs down.
Level 2: Long-lever bridge (more glute)
- Move feet slightly farther away; keep ribs down; stop before back takes over.
3B) Side-lying hip abduction (glute med)

How to do it
- Lie on your side, bottom knee bent, top leg straight.
- Rotate top toes slightly down (targets glute med better).
- Lift the top leg 20–30 cm, pause 1 second, lower slowly.
- Do 2–3 sets of 10–15 reps.
If you get lateral hip pain, reduce range and slow down. Better control often equals less tight glutes and lower back pain.
3C) Step-down control (pelvic stability)
How to do it
- Stand on a step with one foot; the other foot hovers off the edge.
- Slowly bend the standing knee and tap the hovering heel to the floor.
- Keep pelvis level; knee tracks over mid-foot.
- Do 2 sets of 6–10 reps per side.
This is high-value for tight glutes and lower back pain on one side, because it trains single-leg control.
Step 4: Rebuild the hinge (the movement that protects your back)
4A) Dowel hip hinge drill (5 minutes)

How to do it
- Hold a broomstick along your spine: head, mid-back, and tailbone all touching.
- Soften knees.
- Push hips back as if closing a car door with your butt.
- Keep the three contact points. Stop before you lose tailbone contact.
- Do 8–10 slow reps.
When hinge improves, tight glutes and lower back pain during lifting often decreases because the hips share load again.
4B) “Reach to wall” hinge (easier to feel)
Stand ~20–30 cm in front of a wall. Hinge back until your butt touches the wall, then return. Do 2 sets of 6–8 reps. This teaches “hips back” without overthinking.
Step 5: Return to life (habits that stop relapse)
Walking strategy
- Start with a comfortable stride length. If longer steps increase tight glutes and lower back pain, shorten stride and increase cadence slightly.
- Add hills last.
- If one side always tightens first, spend 2–3 minutes on the weaker-side glute med drill before walking.
Sitting strategy
- Stand up every 30–45 minutes for 1–2 minutes.
- Avoid “hanging” on one hip.
- Use a small lumbar roll only if it reduces symptoms; if it increases arching, skip it.
Sleep strategy
- Side sleeping: pillow between knees.
- Back sleeping: pillow under knees.
Avoid stomach sleeping if it increases extension-driven tight glutes and lower back pain.
Do’s and don’ts (the practical guardrails)
Do
- Use small, frequent movement breaks if tight glutes and lower back pain is worse after sitting.
- Train glute endurance (moderate reps, clean form) rather than chasing max strength early.
- Keep exercises below the “nerve irritation line” (no increased tingling, burning, or spreading symptoms).
- Track your triggers for 7 days: sitting time, steps, lifting, sleep, stress.
Don’t
- Don’t force long, painful glute stretches if they rebound symptoms.
- Don’t foam roll aggressively over deep butt pain that reproduces nerve symptoms.
- Don’t jump from zero to high-volume walking/running—capacity mismatches create flare-ups.
- Don’t assume “tight” equals “weak” or “short.” It often equals “protective.”
A simple 2-week plan
Daily (5–10 minutes)
- 90/90 breathing: 5–8 breaths
- Glute isometric set: 6–8 holds
- Hip flexor stretch: 2–3 x 20–30 sec/side
3 days/week (15–25 minutes)
- Bridges: 2–3 x 8–12
- Side-lying abduction: 2–3 x 10–15
- Step-downs: 2 x 6–10/side
- Dowel hinge: 8–10 reps
Track symptoms: tight glutes and lower back pain should become less frequent, less intense, and less “sticky” after sitting or walking.
When to get personalized help
Get assessed if:
- Tight glutes and lower back pain is worsening over 2–3 weeks despite consistency.
- You have persistent leg numbness/tingling or weakness.
- Night pain dominates, or you cannot find any comfortable position.
- Your hip has catching, locking, or significant groin pain.
A clinician can differentiate lumbar, SI, hip, and neural contributions and tailor loading and progression.
FAQ
1) Why do I get tight glutes and lower back pain after sitting?
Sitting puts hips in flexion and often reduces hip extension capacity temporarily. When you stand and walk, your body may borrow extension from the lumbar spine and clamp the glutes for stability, creating tight glutes and lower back pain after sitting.
2) Is tight glutes and lower back pain a sign of sciatica?
It can be, but not always. Butt tightness can occur with disc sensitivity, deep gluteal irritation, SI joint pain, or simple overload. If symptoms travel below the knee, or you have numbness/weakness, get evaluated.
3) Should I stretch if I have tight glutes and lower back pain?
Gentle stretching can help if it does not reproduce nerve symptoms. But if stretching gives only short relief or flares pain, prioritize isometrics and strengthening first—guarding often drives tight glutes and lower back pain.
4) Can weak glutes cause low back pain?
Hip abductor weakness is common in chronic non-specific low back pain populations and improving hip and trunk capacity can improve function and disability.
5) Why is tight glutes and lower back pain on one side so common?
Walking and stairs are single-leg tasks. If one side has poorer pelvic control or hip mobility, the lumbar spine compensates. That produces tight glutes and lower back pain on one side, often with trunk lean or pelvic drop.
6) Is it piriformis syndrome if my butt hurts?
Not automatically. Piriformis syndrome is often over-assumed, and butt pain can come from lumbar referral, SI irritation, hamstring tendon issues, or deep gluteal myofascial pain.
7) What is the “fix most people miss” for tight glutes and lower back pain?
Most people chase deeper stretching. The missed fix is improving hip extension, pelvic control, and glute endurance so the nervous system stops choosing tension.
8) How long does it take for tight glutes and lower back pain to improve?
Many people notice early changes in 1–2 weeks with consistent daily resets and 2–3 strength sessions weekly. Durable change usually takes 6–12 weeks of progressive loading.
9) Can running cause tight glutes and lower back pain?
Yes—especially if stride length increases before hip extension capacity and pelvic control are ready. Build glute endurance and adjust cadence/stride to reduce tight glutes and lower back pain in runners.
10) When is tight glutes and lower back pain serious?
Red flags include bowel/bladder changes, saddle numbness, progressive weakness, fever, unexplained weight loss, or severe trauma. If these exist, seek urgent evaluation.




