Picture this. You stand up after a long meeting, and a sharp twinge clamps across your lower back. It feels random, yet it keeps happening. Understanding what causes lower back pain is the fastest way to break the cycle. In this guide, I explain the real reasons it shows up, how to tell simple strain from something serious, and what you can do today to prevent the next flare.
Most episodes are mechanical and not dangerous. In plain language, what causes lower back pain often comes down to a mismatch between the load you put on your back and the capacity of your tissues to handle that load. Small strains, irritated joints, a grumpy disc or nerve, long sitting, poor sleep, and stress can nudge the system past its limits. When you reduce the load and rebuild capacity, pain becomes less frequent and less intense. Knowing what causes lower back pain helps you take the right next step.

Why low back pain occurs: the short version
- Your spine is strong. Most flares reflect irritated but healable tissues, not “damage.”
- Repeated overload from one or more drivers creates a sensitive “overprotective” pain response.
- Lower the load (in the short term), then nudge capacity higher (in the medium term).
- This cycle explains what causes lower back pain for many office workers, parents, and recreational athletes.
- Red flags are uncommon but important to recognize quickly. We cover those below so you know when to seek care.
How pain actually starts: load versus capacity
Think of your back like a well-trained team. On good days there is plenty of headroom between the weight of your day and the team’s ability to carry it. On rough weeks the margin shrinks. When a long car ride, several nights of poor sleep, a stressful deadline, and an awkward lift stack up, that margin can flip. That is what causes lower back pain seemingly “out of the blue.”
Key ideas that connect to what causes lower back pain:
- Sensitivity rises before structure fails. Pain is a protective alarm. Tissues may be irritated long before there is any structural injury.
- Recovery restores capacity. Sleep, nutrition, and stress management raise the “capacity line,” which is why low back pain occurs less often in well-recovered people.
- Graded loading is medicine. Thoughtful exposure to movement and strength work teaches tissues to handle more without protest, which directly addresses why low back pain occurs during daily tasks.
The usual mechanical suspects that add up
These patterns commonly explain what causes lower back pain in day-to-day life:
1) Small muscle or tendon strains
A rushed yard-work day, a sudden twist, or picking up a sleepy toddler can irritate the paraspinals, gluteal tendons, or hamstrings. Endurance falls, stiffness rises, and the brain turns the alarm up. This is a common example of what causes lower back pain after weekends.
2) Facet joint irritation
Repeated arching or prolonged standing can irritate the small joints at the back of the spine. Bending backward may pinch and bending forward may feel relieving. This pattern is a common reason why low back pain occurs in retail or healthcare workers who stand a lot.
3) Disc-related pain and nerve irritation
Sitting for hours loads the discs in a flexed position. A sensitive disc can protest with a deep ache and occasional leg symptoms. A cough or sneeze may increase pressure. This is a classic reason why low back pain occurs during road trips and long flights.
4) Long sitting with few movement breaks
Your back is designed for variety. Fixed postures reduce blood flow and fatigue supportive muscles. This low-variety pattern often explains what causes lower back pain by mid-afternoon at a desk.
5) Sleep debt and stress
Poor sleep and chronic stress lower your pain threshold and slow recovery. That biochemical context makes it easier for small loads to irritate tissues, which is another reason what causes lower back pain during busy seasons at work.
6) Deconditioning
When glutes and trunk muscles lack endurance, more load shifts to passive structures. That imbalance is a quiet, persistent reason why low back pain occurs during chores, sports, and even standing.
Your lower back is a strong, flexible stack of bones, discs, and joints supported by layers of muscles and ligaments. Different problems create different patterns. Recognizing them helps you connect what causes lower back pain with what you feel.
| Source | What it often feels like | Typical triggers | Try this first | See a clinician now if… |
|---|---|---|---|---|
| Muscle strain or spasm | Tight, sore band across the low back | Sudden lift, twist, new workout | Keep walking, gentle heat or ice, short rest, light core work | Fever, trauma, unrelenting night pain |
| Facet joint irritation | Local ache on one side, worse with arching back | Prolonged standing, sway-back posture | Posture reset, hip hinge practice, anti-inflammatory strategies | Pain down both legs or progressive weakness |
| Disc bulge or herniation | Back pain with leg pain below knee, cough or sit worsens | Long sitting, bending, heavy lift | Relative rest from provoking tasks, gentle walking, gradual extension-bias work | Foot drop, bowel or bladder changes |
| Nerve root irritation (sciatica) | Burning or electric pain down leg, numbness | Disc bulge, stenosis | Nerve glide drills, paced walking, avoid end-range flexion early | Progressive numbness or weakness |
| Spinal stenosis | Leg heaviness or pain with walking, relief when leaning forward | Age-related changes | Flexion-bias exercise, walking program with breaks | Sudden, severe weakness or balance loss |
| Sacroiliac or hip referral | Buttock or outer hip pain that mimics back pain | Pregnancy, one-leg-dominant tasks | Glute strength, load sharing, avoid one-leg sag | Inability to bear weight after a fall |
| Osteoporotic wedge fracture | Sudden, localized pain after minor strain in older adult | Low bone density | Medical evaluation, bracing guidance, fall-proofing | Height loss, multiple recent fractures |
Each pattern points to a different reason for what causes lower back pain, which is why one-size advice rarely works.
Low back pain is one of the most frequent reasons adults seek care and miss work. The CDC’s 2024 National Health Interview Survey data brief reports that 24.3% of U.S. adults had chronic pain and 8.5% had high-impact chronic pain in 2023, with higher rates in women and older adults. These numbers underscore the need to prevent small issues from becoming long-lasting problems. CDC
Global research continues to rank low back pain among the top causes of disability, affecting hundreds of millions of people worldwide and straining economies through medical costs and lost productivity. Estimates place U.S. annual costs related to back pain near $200 billion when you combine direct care and indirect losses. PMC+1
Nerve-related patterns versus muscle-joint patterns
Understanding these differences clarifies what causes lower back pain and what to do next.
| Pattern | What it feels like | What helps early on | What to watch |
|---|---|---|---|
| Muscle or tendon strain | Achy, stiff, sore on movement, better with gentle motion | Short walking breaks, light heat, easy range-of-motion | Rapid spikes in activity that re-irritate |
| Facet irritation | Pinch with extension, relief with flexion | Hip hinge habits, avoid deep sway-back standing, short trunk endurance work | Standing all day without breaks |
| Disc-related pain ± radicular symptoms | Deeper ache, worse with prolonged sitting, may have leg pain | Frequent position changes, gradual extension bias or neutral spine work | Progressive numbness, weakness, bowel or bladder changes (seek care) |
The table above captures many of the key factors behind what causes lower back pain in daily life and how simple changes can help.
When it is not just mechanical: red flags you should not ignore
Serious causes are rare but important. Seek urgent medical care if back pain is accompanied by any of the following:
- New bowel or bladder trouble
- Progressive weakness, numbness, or tingling in a leg
- Fever, unexplained weight loss, or pain after significant trauma
- Pain that is constant or wakes you at night
Knowing the red flags helps you act promptly, which is essential even as you build a plan around why low back pain occurs most of the time.
Do you really need a scan?
Most uncomplicated acute low back pain does not need imaging at first. In the absence of red flags, time and graded activity tend to outperform early scans. The U.S. National Library of Medicine’s patient page explains that MRI is typically reserved for cases with specific warning signs like severe neurological changes.
This avoids incidental findings that do not change care and adds clarity to what causes lower back pain without rushing into expensive tests.
What evidence says about early management
- Keep moving within tolerance. Evidence syntheses show bed rest is not more effective than staying active for acute low back pain and may delay recovery in some cases. [The Updated Cochrane Review of Bed Rest for Low Back Pain and Sciatica, 2005]
- Education works. Clear explanations that connect symptoms to load and capacity help people make better choices, which is why low back pain occurs less often after people learn how to self-manage flares.
- Graded exercise beats passive care alone. Building endurance and strength raises capacity so daily loads feel lighter.
- Sleep is a treatment multiplier. Recovery enhances every other input and is often the missing piece in why low back pain occurs repeatedly.
The prevention “priority stack” you can actually follow
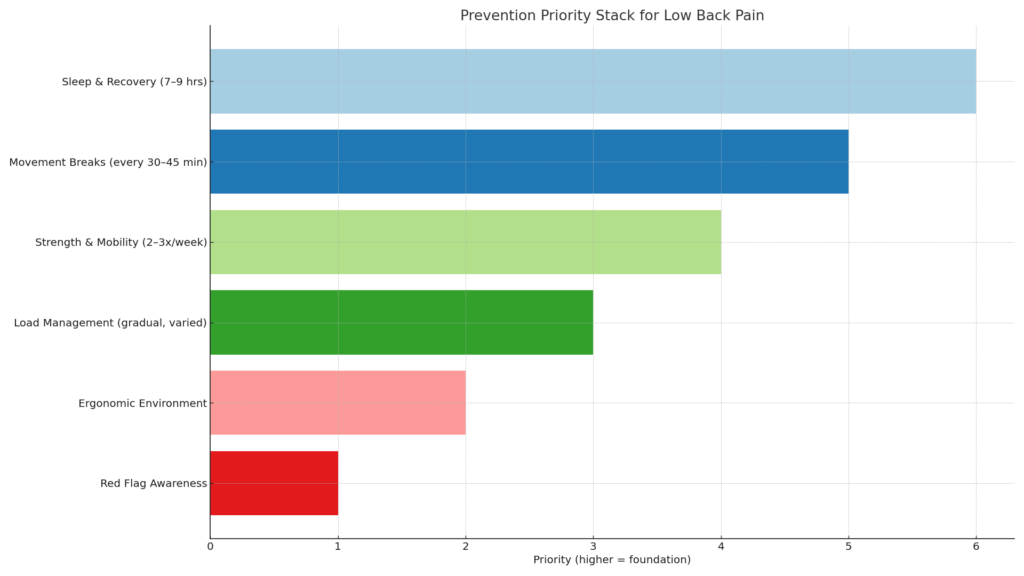
Sleep and recovery
Aim for a regular 7 to 9 hours. Keep your wake time consistent, cut caffeine after lunch, and dim screens 60 minutes before bed. Rest raises tissue capacity and reduces sensitivity, which is central to why low back pain occurs less frequently.
Movement breaks
Set a gentle timer for every 30 to 45 minutes. Stand, walk to the printer, do five calf raises, or perform three hip hinges. Variety at the spine matters. This is a simple reason why low back pain occurs less when you sprinkle movement into your day.
👨⚕️ Dr. Arora’s Clinical Note:
A common mistake people make with “movement breaks” is doing them too rarely and too aggressively—then blaming the chair when the back flares again. A more reliable strategy is micro-unloading: tiny, frequent resets that calm disc/joint pressure and re-engage the hip hinge pattern before stiffness “locks in.”
Try the 20–20 reset (2–3 workdays in a row): every ~20 minutes of sitting, stand for 20 seconds and do 3 slow hip hinges (hands on thighs, push hips back, neutral spine) + 2 deep nasal breaths. This often outperforms a single big stretch once an hour.
Quick “direction test” to personalize your break:
- If 5 gentle standing back-bends (hands on hips, small range) makes pain feel more centered or easier, you likely tolerate an extension-bias reset.
- If back-bends feel worse or you get leg heaviness (stenosis-like pattern), use a forward-lean reset instead (hands on desk, slight hip hinge for 10–15 seconds).
The goal is not perfect posture—it’s frequent pressure changes + better loading mechanics so your back stops needing to “shout” by mid-afternoon.
Strength and mobility
Two to three sessions per week are a solid target. Use a mix of:
- Hip hinge work: Romanian deadlift pattern with light dumbbells
- Anti-rotation core work: dead-bugs, suitcase carry
- Glute endurance: bridges or hip thrusts, step-ups
- Mobility “snacks”: cat-camel, open books, hip flexor stretch
This builds capacity and reduces the frequency of why low back pain occurs under normal chores and sport.
Load management
Increase total training or yard-work load by about 10 to 20 percent per week, not 100 percent in a weekend. Rotate tasks. Do not combine your heaviest lifting day with the longest sitting day if you can help it. These simple rules cut down why low back pain occurs after big pushes.
Work setup that respects your spine
- Chair height: hips slightly higher than knees
- Feet flat or supported
- Screen at eye level
- Keyboard and mouse close so elbows stay near the body
- Option to stand for 10 minutes each hour
A comfortable setup reduces the reasons why low back pain occurs during long projects.
A 7-day reset plan to calm a flare and build momentum
This plan is for uncomplicated mechanical pain without red flags.
Day 1–2: Calm the system
- Short walks every few hours
- 2 to 3 sessions of easy mobility: pelvic tilts, knee-to-chest, cat-camel
- Light heat for 10 minutes if it feels good
- Bed rest is not advised; keep moving within tolerance. This early approach addresses why low back pain occurs after overdoing it.
Day 3–4: Restore confidence
- Add 2 sets of bodyweight hip hinges and bridges
- 5-minute breathing drill before bed
- Keep the walk habit
- Reduce sitting bouts to less than 45 minutes, which tackles a common reason why low back pain occurs in desk workers.
Day 5–7: Build capacity
- 3 sets of goblet squats with light weight if available
- 3 sets of suitcase carry for 30 seconds per side
- Gentle return to normal tasks with pacing
- End each day with two minutes of spine-friendly mobility
- The steady build explains why low back pain occurs less often as the weeks go by.
What about medications and procedures?
- Over-the-counter options like acetaminophen or nonsteroidal anti-inflammatory drugs can help in short courses for flares.
- Injections and surgeries are reserved for select cases after a period of rehabilitation and only when specific criteria are met. Most people improve without them, which is another reason why low back pain occurs less often when you lean on education and exercise first.
- Physical therapy helps you identify your drivers, correct movement habits, and progress loading safely. That knowledge reduces the chances of what causes lower back pain flaring up again.
Putting it all together
- Recognize the drivers that explain what causes lower back pain for you.
- Adjust the load this week and rebuild capacity over the next four to eight weeks.
- Watch for red flags and get help promptly if they appear.
- Use a prevention priority stack so wins accumulate even when life is busy.
Why low back pain occurs at different ages
Teens and 20s. Sports overload, deconditioning, and long study hours explain what causes lower back pain here. Guidance focuses on technique and basic strength.
30s and 40s. Work sitting and child care lifting add up. The fix is better ergonomics, movement snacks, and consistent walking.
50s and 60s. Stiff hips and spinal arthritis creep in. Understanding stenosis patterns clarifies what causes lower back pain, and a flexion-friendly walking plan helps.
70s and beyond. Bone health matters more. Gentle strength work and balance training prevent falls and reduce the risk that a small incident becomes a painful fracture.
Programming your week for prevention
Here is a simple template you can adapt once you know what causes lower back pain in your case.
- Daily: 20 to 30 minutes brisk walking, posture resets each hour you sit
- Twice weekly: Glute bridges or hip thrusts, bird dog, side plank variants, farmer’s carry
- Once weekly: Hip hinge practice with a light kettlebell, suitcase carry, step-ups
- As needed: Short heat or ice, self-massage with a ball, relaxing breath work
Progress slowly. Your goal is consistency, not pain-provoking hero workouts.
When to seek a second opinion
If you have persistent leg symptoms, progressive weakness, or if you are simply not improving after several weeks despite following a good plan, consult a clinician who treats spine conditions regularly. Clear tests and a targeted progression can change the answer to why low back pain occurs for you.
Conclusion
There is rarely one single villain. For most people, what causes lower back pain comes down to how the spine is moved, loaded, and supported in daily life. The big wins are simple: keep walking, break up long sits, build hip and core strength, and use imaging only when it changes care. If symptoms persist or serious signs appear, get a professional evaluation. With the right plan, you can reduce the chances of what causes lower back pain and keep doing the things you enjoy.
Frequently Asked Questions
Why does my back hurt after long sitting?
Sitting for long periods reduces blood flow and tires the supporting muscles. Taking short breaks to stand or walk helps relieve this.
Should I rest completely during a back pain flare?
Complete bed rest is rarely recommended. Gentle movement usually helps you recover faster, while long rest periods can slow healing.
Do I always need an MRI for back pain?
Not at first. MRI is only advised if there are red flag symptoms or if pain and neurological issues persist despite care.
What are the red flags for back pain?
Seek urgent medical care if you notice new bladder or bowel problems, progressive leg weakness, fever, unexplained weight loss, or pain after major trauma.
Can stress make back pain worse?
Yes. Stress and poor sleep reduce your body’s ability to handle discomfort, making flare-ups more frequent and recovery slower.
Which exercises help the most for back health?
Hip hinges, glute bridges, planks, and progressive strength training are effective for building resilience and reducing future flare-ups.
How quickly should I increase activity after pain?
Increase activity gradually, around 10–20% per week. Sudden jumps in intensity or duration can trigger new symptoms.
Does posture really matter?
Yes, but variety matters more than one perfect posture. Switching positions often is more protective than holding a single fixed pose.
When is surgery considered for low back pain?
Surgery is considered only in specific situations, such as severe nerve compression, spinal instability, or when conservative treatments fail.
How long do typical back pain flares last?
Most episodes improve within a few weeks if you stay active and pace daily tasks. Strengthening the trunk and hips reduces recurrence.




