If you’ve recently had a Spinal stenosis MRI and the report mentions terms like “narrowing” or “compression,” it’s natural to feel alarmed. You’re not alone—many people discover spinal stenosis unexpectedly after an MRI scan for back or neck pain. The key is to understand what it means, what your options are, and how you can manage it effectively, often without surgery. This article is your detailed, expert-backed guide to navigating life after a diagnosis of spinal stenosis on MRI.

What Does “Spinal Stenosis on MRI” Mean?
So, your MRI just dropped the bomb: it shows spinal stenosis. Sounds scary, right? But don’t panic just yet.
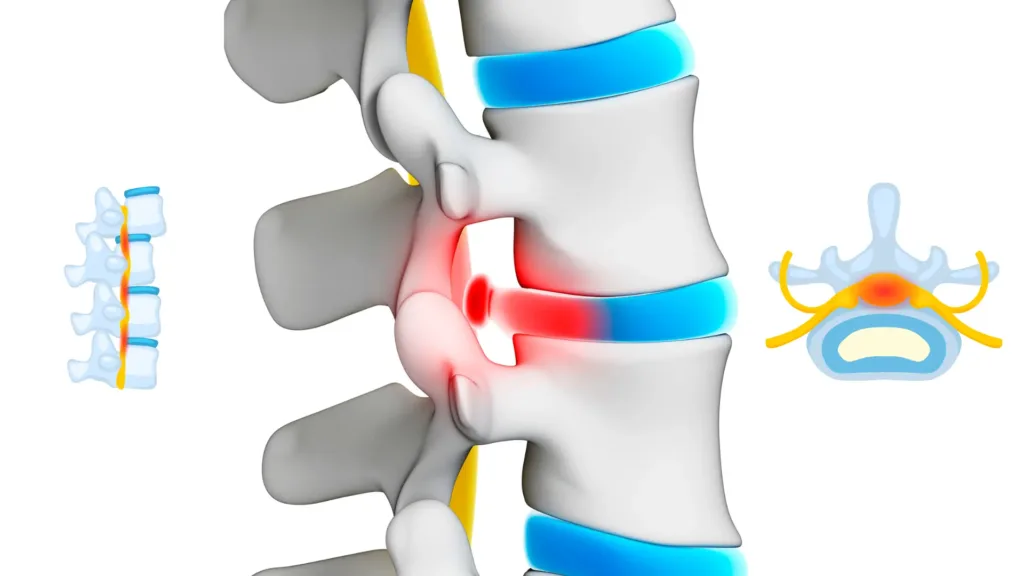
At its core, spinal stenosis on MRI means that the open spaces within your spine—either the central canal or the small openings where nerves exit—are narrowing. This narrowing can compress the spinal cord or nerves, which may cause pain, numbness, or other symptoms. However, the condition ranges from mild and manageable to more severe. Not all stenosis requires aggressive intervention.
Think of your spine like a highway. Spinal stenosis is like a traffic jam—things are still moving, but slower, and sometimes the pressure builds up in specific lanes (nerves).
Types of Spinal Stenosis
Lumbar Spinal Stenosis
This is the most common type and affects the lower back. It can cause:
- Pain radiating down the legs (sciatica-like symptoms)
- Tingling or numbness in feet or calves
- Leg fatigue or heaviness when walking or standing
- Relief when leaning forward or sitting down (shopping cart sign)
It often limits walking distance and can mimic peripheral vascular disease, so a thorough diagnosis is essential.
Cervical Spinal Stenosis
This affects the neck region and can be more serious. Why?
Because your spinal cord passes through the cervical spine. If it’s compressed, symptoms can involve:
- Neck pain with radiating arm symptoms
- Loss of hand dexterity
- Balance issues
- In severe cases, weakness or paralysis
This type of stenosis deserves prompt evaluation and management.
Causes of Spinal Stenosis
A Spinal stenosis MRI typically reveals one or more of the following culprits:
- Aging: Natural wear-and-tear leads to degeneration of discs, joints, and ligaments
- Herniated Discs: Discs that bulge or rupture may intrude into the spinal canal
- Bone Spurs (Osteophytes): Extra bone growths can reduce space in the canal
- Thickened Ligaments: Ligaments like the ligamentum flavum may stiffen and thicken
- Spinal Injuries: Fractures or trauma can shift bone or cause swelling
- Congenital Conditions: Some people are born with a naturally narrower canal
Understanding the root cause helps guide your treatment and prognosis.
Risk Factors You Should Know
You’re more likely to be diagnosed with spinal stenosis on MRI if:
- You’re over 50 years old
- Have osteoarthritis or rheumatoid arthritis
- Lead a sedentary lifestyle
- Are overweight
- Have had prior spinal surgery or injuries
That said, younger individuals—especially athletes and those with heavy lifting jobs—are not immune, especially if structural changes exist from previous injuries or congenital narrowing.
Decoding Your Spinal Stenosis On MRI Report
What Does the Radiologist’s Language Really Mean?
An MRI report can seem like it’s written in another language. Let’s decode some common phrases seen in Spinal stenosis MRI results:
- “Central canal narrowing at L4-L5”: The main tunnel for your spinal cord is tight at the L4-L5 vertebral level (lower back).
- “Mild foraminal stenosis on the right”: Nerve passageways (foramina) are narrowed, possibly pinching nerve roots.
- “Disc bulge with facet hypertrophy”: The disc is protruding, and the small joints in the spine are enlarged from degeneration.
These terms help determine the severity and location of your stenosis, which in turn influences treatment planning.
Common Terms in MRI Reports
- Degenerative Disc Disease: Age-related disc changes, often seen by age 30-40.
- Disc Bulge: A disc is pushing out but not ruptured.
- Facet Joint Arthropathy: Arthritis of spine joints causing pain and stiffness.
- Foraminal Narrowing: Openings where nerves exit are reduced in size.
The key point? Many people have these findings even without pain. Your Spinal stenosis MRI must be correlated with symptoms to decide next steps.
When Should You Be Concerned?
Not every case of spinal stenosis is urgent, but here’s when to act:
- Moderate to severe narrowing (especially with nerve compression)
- Persistent or worsening pain
- Difficulty walking, numbness, or weakness
Ignoring symptoms can lead to long-term nerve damage or functional loss.
Symptoms You May Be Feeling
Early-Stage Signs
- Aching in lower back or neck
- Occasional tingling in arms or legs
- Subtle weakness when climbing stairs or gripping objects
Progressed Symptoms
- Cramping in calves or thighs after walking (neurogenic claudication)
- Pain that improves when bending forward or sitting
- Gait imbalance or frequent stumbling
Emergency Red Flags
These warrant an immediate ER visit:
- Sudden loss of bladder or bowel control
- Inability to move a limb
- Sharp drop in coordination or severe numbness
What Happens Next?
Do All Spinal Stenosis On MRI Results Require Surgery?
Absolutely not.
A Spinal stenosis on MRI is just one tool. Many people live symptom-free or with mild symptoms for years without surgery. Conservative care is the first step in most cases.
Who Should You See First If You See Spinal Stenosis On MRI: Neurologist, Orthopedist, or Physio?
Here’s a smart sequence:
- Physiatrist (non-surgical spine specialist)
- Physiotherapist (for customized rehab plan)
- Orthopedic or Neurosurgeon (if symptoms progress or fail to improve)
The key is team-based care. One-size-fits-all rarely works with spinal issues.
Getting a Second Opinion
Always wise, especially when:
- Surgery is suggested early
- You’re unsure about diagnosis
- Symptoms don’t align with MRI findings
A second (or third) set of eyes ensures you’re not missing safer, effective options.
Non-Surgical Management Options
Lifestyle Modifications
- Posture correction: Use lumbar support, adjust screen height
- Movement breaks: Avoid prolonged sitting or standing
- Weight management: Reduces spinal load
- Sleep hygiene: Use supportive pillows; back sleeping with knee elevation is ideal
Small daily changes make a big long-term difference.
Physical Therapy and Exercise
Working with a physiotherapist can drastically improve symptoms. Recommended approaches include:
- Core stability training
- Pelvic tilt exercises
- Isometric strengthening
- Hamstring and hip flexor stretches
Avoid:
- Deep forward bends
- Twisting exercises
- High-impact cardio (like running)
Instead, try stationary biking, walking on an incline, or aquatic therapy.
👨⚕️ Dr. Arora’s Clinical Note:
A common mistake I see is turning the “shopping cart sign” into a full-day posture strategy—because the short-term relief is so convincing. Clinically, that advice is incomplete. Yes—gentle flexion often reduces leg symptoms (the classic “shopping cart” relief), but the mistake is living in a constant slumped position all day. That can decondition the trunk and hips, stiffen the thoracic spine, and make walking tolerance worse over time.A more reliable approach is the “Flexion Sweet Spot + Capacity Build” rule:
- Use flexion as a symptom tool, not a posture. Do short resets (30–60 seconds) of supported forward-lean or a brief sit break only when symptoms start.
- Then build capacity in the hips and trunk (glutes + core endurance) so your spine doesn’t take the full load. Often, improving hip extension strength reduces the “back doing everything” pattern that fuels stenosis flare-ups.
- Try this quick self-check: Walk 3 minutes upright, note symptoms; then walk 3 minutes with a slight forward lean (hands on thighs or a treadmill rail). If the lean gives clear relief, you likely benefit from interval walking (walk until symptoms begin → 30–60 sec lean/reset → repeat) rather than long continuous walks that flare you.
If you notice new or worsening leg weakness, foot drop, numbness that spreads quickly, or bowel/bladder changes, stop self-management and seek urgent medical evaluation.
Pain Management with Medications
Common pharmacological options:
- NSAIDs: Ibuprofen, naproxen—for inflammation
- Muscle relaxants: For spasms
- Neuropathic pain agents: Gabapentin or pregabalin target nerve pain
These are not long-term fixes but can ease symptoms during rehab phases.
Epidural Steroid Injections – Pros & Cons
Pros:
- Often provide fast relief (especially leg symptoms)
- Allow participation in physical therapy
Cons:
- Temporary (effects last weeks to months)
- Risk of complications with repeated use
- Not effective for all patients
Discuss timing and frequency with a pain management specialist.
When Surgery Becomes Necessary
Surgery is typically considered when:
- Conservative care fails
- Neurological deficits develop (e.g., weakness, foot drop)
- Daily life is significantly limited
Surgical Options Available
- Laminectomy: Removes part of the vertebra (lamina) to relieve pressure
- Discectomy: Removes herniated disc material
- Spinal Fusion: Stabilizes vertebrae by joining them together
Each has pros and cons depending on your age, level of stenosis, and health.
Recovery Time and Expectations
- Minimally invasive procedures: Resume light activity in 2–6 weeks
- Fusion surgeries: May need 3–6 months of supervised rehab
Physiotherapy post-op ensures you regain strength and mobility safely.
Minimally Invasive Surgeries
These newer techniques offer:
- Shorter hospital stays
- Smaller incisions
- Less blood loss
- Faster recovery
Always ask your surgeon if you’re a candidate.
Living With Spinal Stenosis
Daily Tips for Comfort
- Use supportive seating with lumbar rolls
- Take standing/walking breaks every 30–60 minutes
- Heat therapy: Warm baths, hot packs can ease muscle tension
Exercises to Avoid
- Deadlifts and squats with weight
- Sit-ups or crunches
- Golf swings or other twisting motions
Focus instead on safe strengthening and flexibility routines guided by a physiotherapist.
Long-Term Outlook
The good news? Most people with spinal stenosis live full, active lives.
Key takeaways:
- Don’t delay early treatment
- Build spinal strength and flexibility
- Monitor changes and consult professionals
Consistency wins over quick fixes.
Conclusion
Receiving a Spinal stenosis on MRI report can feel overwhelming, but remember—this isn’t a sentence, it’s a signal. Most cases can be managed without surgery through smart choices, guided physiotherapy, and informed lifestyle changes.
Your spine is your foundation—treat it with care, get professional guidance, and take charge of your recovery. With early intervention and a well-rounded plan, you can keep moving forward—comfortably and confidently.
FAQs
1. Is spinal stenosis on MRI curable without surgery?
Not curable, but absolutely manageable with therapy, posture correction, and medication.
2. How long can you live with spinal stenosis?
A full, healthy life—most people don’t need surgery.
3. What worsens spinal stenosis?
Poor posture, inactivity, weight gain, and ignoring early symptoms.
4. Can spinal stenosis go away on its own?
The narrowing stays, but symptoms can improve or stabilize.
5. What sleeping position is best for spinal stenosis?
Back sleeping with knees slightly elevated or side sleeping with a pillow between the knees.
6. Is spinal stenosis a form of arthritis?
It often results from arthritis but is not itself arthritis.
7. Is walking good for spinal stenosis?
Yes! Especially on flat surfaces with short, frequent intervals.
8. What’s the difference between spinal stenosis and a herniated disc?
A herniated disc is one cause of spinal stenosis—stenosis is the result of narrowed spaces.
9. Are epidural injections safe for spinal stenosis?
Generally safe when done by specialists, but effects may be temporary.
10. Can physiotherapy really help spinal stenosis?
Yes, especially when personalized and consistent—it’s a cornerstone of non-surgical care.
With 20+ years of clinical experience in spine, joint, and pain management, Dr. Vivek ensures every article reflects accurate, trustworthy, and up-to-date health advice.
Learn more about Dr. Vivek’s qualifications & journey →




